April 2, 2021
Facebook Live: Hormones, Misconceptions, and Cognition
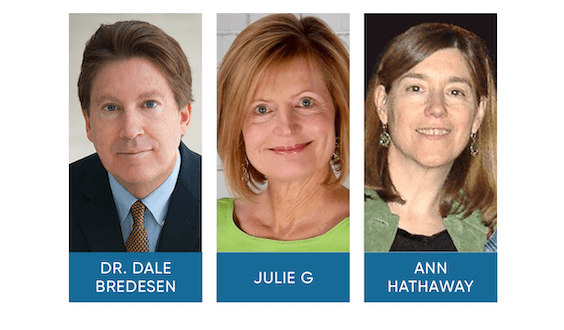
Apollo Health’s Dr. Dale Bredesen, Chief Science Officer, and Julie Gregory, Chief Health Liaison, and Dr. Ann Hathaway participated in a Facebook Live session, “Hormones, Misconceptions, and Cognition.” As a courtesy we have included a full transcript of the session below the video.
Watch here:
Full Transcript:
Dr. Bredesen: Okay. Hi everybody. Welcome, I hope everyone’s doing very well. I’m so honored today to have a real expert on bioidentical hormones, Dr. Anne Hathaway, and thanks so much for joining us today.
Dr. Hathaway: Very happy to be here with you Dale. Thanks.
Dr. Bredesen: And we also have Julie G who has experience with bioidentical hormones. So we really have both sides cover here with a real expert, clinician as well as someone who had has experienced with firsthand experience with using these. One of the most common questions we’re asked is what do hormones have to do with cognition? How do I use them? Is there a problem? Are there side effects? I’m concerned about it? My doctor does it use them on and on and on, so we hear an awful lot about bio identical hormones and how important they are in cognition. So we thought it would be really helpful to bring in a real expert like Dr. Hathaway. So Ann, let’s start with some basics here. How important is it to have optimal hormone status for cognition?
Dr. Hathaway: It is of critical importance. Absolutely. The brain is full of estrogen receptors, tremendous density of estrogen receptors and those parts of the brain that deteriorate in Alzheimer’s disease have the highest density of estrogen receptors. And we’ve seen in my work, in much of the research, that estrogen has a tremendous, tremendously strong impact on brain health, Whitney Wharton in her seminal 2009 paper believes that if all women were started on estrogen at the time of menopause, we would decrease Alzheimer’s disease by at least 34%. And I certainly believe that that is true. Yeah. But the problem is, you know, when you think about hormones and you try and look at all the research you can feel like you’re in an upside-down world. Because the women’s health initiative said the exact opposite, and it’s really complex to explain why that’s the case, right? The Women’s Health Initiative changed everything; about the way we look at hormones in 2002. And some of what they said was right and some of what they said was very very wrong and they’ve revised and revised and revised. So it’s really hard. I have people sending me research all the time like, Ann, what about this research? What about that research? It says the opposite of what you’re saying and that’s the problem. The problem is which hormone you choose and the way you deliver it is incredibly important. When you use estrogen, you wanna only use estradiol and you only wanna use it on the skin, a creamer patch. That’s the optimal estrogen. When you’re using a progesterone, which you need to do, if you’re giving a woman estrogen and she has uterus because estrogen grows the uterine lining and that can cause problems. But when you use a progesterone you can’t use Medroxyprogesterone or Norethindrone, one of these synthetics. They have negatives, whereas real progesterone, although you know, you can fine tune it and it can cause a little bit of issue in some women. Overall, real progesterone has really positive effects on the brain, on sleep. It protects from vascular damage as does estrogen. So that’s kind of the basics and the reason why things are so confusing the Women’s Health Initiative used you can’t fault the Women’s Health Initiative because they use the hormones that were being used by almost all gynecologists at the time. Oral estrogen in the form of Premarin has some positives and some negatives. Medroxyprogesterone synthetic progesterone that we use, almost completely negative. Causes bone loss, decreases the action of mighta the upregulation of our mitochondria, the energy source in the brain, estrogen increases that, Medroxyprogesterone will reverse that. And on and on Medroxyprogesterone has negative cardiovascular effects almost every category that you look at the synthetic progestin that was used has negatives. And when you look at the medical literature, the big, big problem there is that in the synopsis, in the title, in the abstract you won’t know what estrogen they used, what form and what progesterone they used. They’ll use progesterone the word progesterone when they use a synthetic. So that’s why we have such a problem with, you know getting clarity on this topic.
Dr. Bredesen: So for perspective then, what you pointed out about how much it could be, dementia could be reduced. If you translate that to how many of the currently living Americans are slated to develop Alzheimer’s disease, if we are not successful with prevention, that’s translating to about 15 million, fewer cases of the currently living 330 or so million Americans of dementia. So this is a huge, huge impact, and I know Julie, let’s talk to you for just a second here I know you have as part of your overall protocol included BHRT and have actually changed it over the course of time. Did you notice changes when you increased your estradiol levels and when you went on optimal BHRT yourself?
Julie Gregory: I did. I ended up having pretty abrupt onset of menopause and it was pretty traumatic. I had a large fibroid and I had it embolized, and during that procedure, I think the blood supply to my ovaries was cut off, so several weeks later I was essentially normal perimenopause normal. And the next day I was having hot flushes about a dozen an hour. And, these weren’t mild by any means. I mean, I was drenched in sweat and I was completely unprepared for this. And when they would come on at the time I was experiencing mass cell activation I had this sense of foreboding. Like I thought, am I gonna have anaphylaxis? I mean, I really, I couldn’t figure out what was about to happen. And then I would just get extraordinarily ill, sweaty and hot. I would just feel awful. So I went from being normal one day to obviously I had a very abrupt drop in estradiol and I got to see my gynecologist fairly quickly. Thank goodness. And I was put on hormone replacement therapy. At the time It wasn’t bioidentical, unfortunately it was a product called Combipatch, I am inspired among your that. I think it the estrogen may be bioidentical, but the progestin was synthetic. So it was a suboptimal product for sure but it completely rescued me none VLS. And luckily, several months later I switched to a different gynecologist and I got on a more optimized program. Yeah, and then you had recommended that I increase my levels because my levels even with of the patch were still pretty low and increasing them to a point has been helpful for me. I keep my levels probably lower than what both of you would recommend, but it works for me. I think I’m somewhere around 50 and I seem to be doing very, very well there. Energetically my brain feels very stable, as long as I’m on this routine.
Dr. Bredesen: Yeah. And of course, you’re doing many many other things right? So that optimizes. So Ann, let’s talk about levels. What do you usually recommend for your patients with cognitive decline or risk for decline?
Dr. Hathaway: I like to get the estrogen up to at least 45. we don’t have an answer in the literature. There’s no medical literature that’s really looked at. Okay. Let’s think about the brain and optimizing cognitive function long-term, what’s the optimal level. If a woman tolerates a level at 60 or 80 or a 100, that may be optimal, and I do have some women who keep their estrogen at that level. Now measuring estrogen in the blood is a little bit tricky in that you have to kind of time it, right? The last time you put the cream on or in the middle of your patch if you use the patch. Most common bioidentical estrogens that my patients use would be either the patch or some kind of a gel or cream. So for the gel or cream, I like to get a 12 hour level. So you’re right at the mid-point, right? And saying for the patch I like to get it in the middle of the patch. And then you know that because estrogen is processed in the body fairly quickly, it has a 24 to 36 hours half-life so, you know it’s something that you need to keep up constantly. So somewhere between 45 and 100 would be the range that I would choose for and the younger the woman, so the closer she is to having gone through menopause, the higher I will trend in terms of that level. So women in their 50s, I would trend towards taking them up to 80. You do run into some problems with some women of breast tenderness when you start estrogen that’s usually women who’ve been off it for a long time and if I get a lot of questions from practitioners about that. And what I, you know, if you can’t get a woman in her 60s or 70s up over 25 or so at first I would just leave her there for a while and then very gradually try and get her up to maybe 40, 45 because you wanna avoid these side effects because obviously because people are miserable and it’s not gonna encourage them to continue therapy. So 45, 45 to a 100 there’s research that shows that for osteoporosis, a level of 80 gives optimal regrowth of bone. And by the way there’s no medication, that’s ever been created that regrows bone. Estrogen will increase, I’ve seen a 12% increase in bone mass over a four-year period, in some of my patients.
Dr. Bredesen: So one of the most common questions that we get is, okay I have went through menopause at 50, for example and now I’m 62 and beginning cognitive decline. Aren’t I too late to start? so what do you recommend to people who come to see you who have had more than 10 years without but now are suffering some degree of cognitive decline?
Dr. Hathaway: Yeah. So you’ll see in the literature the so-called timing hypothesis, which says that if a woman is within 10 years of menopause, it’s fine, you’re okay to start hormones. But if she’s beyond that you get potentially negative effects from starting hormones. And again, that information is based primarily on the Women’s Health Initiative study, where they used oral Premarin, Premarin for pregnant mare’s urine and a synthetic progestin. And in that study women between age 50 and 59, who started even those you know, what we consider to be very much inferior hormones had all caused mortality decrease. Whereas the older women who were put on those hormones didn’t do as well. So oral estrogen, I said earlier has some positives and some negatives, for example, the Leisure World Study which is an observational study not as good as a placebo controlled, et cetera but in that observational study, where they looked at medical records, they saw that the women who had been on Premarin, for any period of time had a decrease in Alzheimer’s risk. And if they’ve been on Premarin for seven years or more they had a 50% decrease risk of having dementia as a diagnosis on their death certificate was very very significant information. So why is that so different than what the Women’s Health Initiative showed us? And that’s because in my opinion, the dementia studies in the Women’s Health Initiative, they started all the women on Premarin and Provera over age 65. When you start women, who’ve had a chance to develop atherosclerosis of the heart and damage to the brain because of lack of estrogen, and then you put them on Premarin which increases coagulation. It tends to increase blood clotting increases CRP, which we talk about a lot, which is an inflammatory marker and increases fibrinogen, which is a clotting factor. And that’s why when you have a woman who’s been without estrogen for a long period of time you don’t wanna give her oral estrogen, but topical estrogen hasn’t been well studied. And all the studies that we do have suggest that topical estrogen has a massive number of beneficial vascular effects, vascular benefits for the brain, vascular benefits for the heart in the peripheral circulation. And when you’re using a real progesterone, you get added benefits. So I try women of any age. on bio-identical topical estradiol and real progesterone. You have to counsel them carefully and you have to go to a provider who has experience with that. But I do believe that there’s enough evidence to say that it is safe to, number one continue women on hormones, because many doctors say you should discontinue when you’re somewhere between age 60 and 65. The evidence now definitely supports continuation, according to the North American Menopause Society their 2017, four long papers. If you have a woman on topical estradiol and a real progesterone and they’re doing well on the hormones the evidence does strongly support continuation. I had a woman, a patient of mine come to me this week who said, she’s aged 63. She said, my gynecologist said what’s my plan for getting off hormones. And I said, do you think you’re doing well on the hormones? She says, absolutely I love my hormones. So I feel my mood is better, I sleep better, I feel stronger, I can exercise more efficiently on and on. I said, well, the evidence supports continuation for women who are doing well on hormones. And we don’t have, you know the strong evidence that we should have for whether you can start women on hormones. But because in a situation where someone has cognitive impairment, estradiol is so so important. I do start them on hormones, with a lot of care and caution. And most of those women do extremely well on hormones. They get significant cognitive benefits. And, you know, just to add onto that, I can’t tell you maybe eight or nine times in my practice I’ve had women come to me for cognitive impairment, who say my cognitive impairments started when I was on an aromatase inhibitor, for breast cancer. And what an aromatase inhibitor does is it takes your estrogen, that small amount that you have postmenopausal, and it goes like that, takes it to zero. So I do start women, I have a lot of experience with that. And you know, you do need to someone to see someone who’s experienced if you’re gonna to be starting hormones and it’s longer than 10 years after, you’ve gone through menopause.
Dr. Bredesen: Great. Thank you. So the fantastic questions coming through here, let’s go through some of these, First one here is what about estradiol cream for treatment of atrial fib vaginitis if I use that twice a week am I getting estrogen into my bloodstream?
Dr. Hathaway: Yes. If you’re using estradiol vaginally, it’s quite well absorbed, vaginally, and you do get some systemic effect, twice a week is probably not enough, because estrogen is continually in and out of the body. I traditionally use estriol for, for a trophic vaginitis. Now we’re supposed to call it genital urinary syndrome, but, in estriol which is a weak estrogen. Systemically is a strong estrogen on the vaginal tissue, and we’ll treat that dryness problem extremely efficiently. I mentioned, I always use estradiol on the skin. Most of the time I have women put it on their inner arms, but occasionally some women just don’t get good absorption there. And then if you do use estradiol right at the opening at the vaginal opening, you will get very, very good absorption, that tissue is, very effective, absorptive tissue
Dr. Bredesen: Yeah, then there’s a question about ten years into menopause, what can I do? and I think you’ve already answered that very nicely that’s still appropriate. And then a follow-up from Wendy, a physician has me on 75 milligrams of pregnenolone. Should I continue this? So do you usually keep people on pregnenolone or do you usually take them off the pregnenolone when you’re doing the BHRT?
Dr. Hathaway: No, I typically support women’s all hormones. If they’re low in pregnenolone, I will give them pregnenolone. I like to have the level that at least 100. I see many, I always check pregnenolone. I see many post-menopausal women whose pregnenolone is below ten, unmeasurable. Right, so I will support DAGA. I will support pregnenolone, I will support testosterone, estrogen and progesterone. Yeah.
Dr. Bredesen: And then Julie, do you yourself include pregnenolone and or DAGA in your overall approach or are you specifically sticking with estradiol and progesterone?
Julie Gregory: I am not including those, because my blood levels are in the good range, so I don’t seem to have their need.
Dr. Bredesen: Fantastic. Okay. Then the next one here. Let’s see. Okay. What about estradialysis from Donna? What about estradiol cream used directly on the skin and is prometrium natural progesterone also, what do you recommend?
Dr. Hathaway: Yes. Estradiol directly on the skin. That is how we always use it. The tissue, you tend to have good absorption, here from the inner arm. Some women place it, all across the inner arm, I like to avoid using the hand, so I typically have people use a syringe without a needle to put it on, and then rub their two arms together, so then you don’t have to waste any on your hands or wash your hands. You do wanna be careful, after you put the estrogen on, not to transfer it to young children, pets, your husband, et cetera. So that is something to be aware of. And then there was another part to the question.
Dr. Bredesen: Yeah. Well, one of the things I was gonna ask before we go on to the other part here, some people absorb better than others, of course. And for some people transvaginal works, I know Wendy Ellis worked with Jonathan Wright in the past. Very, very, very positive about the idea of transvaginal, especially the transdermal. I know we’ve seen some people where the transdermal doesn’t work very well, and they don’t bother to check the levels and their cognition is not improving. So you’ve gotta go back and make sure that you actually are achieving the levels that you had talked about and that Juliet talked about earlier. So, okay. So for people who are not absorbing well, do you recommend a different product? Or do you recommend going to transvaginal?
Dr. Hathaway: Yes. I always check levels, giving the same person, giving different people the same dose of estradiol, or progesterone for that matter. You do not get the same results. So it is critically important to check blood levels. Some people like to check levels in dry urine. Some people like to check levels and saliva. I’ve always used blood, the medical literature, it has more information, not enough but it has a lot more information on blood levels. So that’s why I’ve liked using blood levels. So yeah, if you’re not getting good blood levels you can increase the dose a bit, or you can switch to a vaginal delivery because it is much easier to get a higher blood level using the vaginal tissue, it’s just more absorptive. Some people don’t want the inconvenience of having to use it that way. And so, you know, you can tailor this a lot to your patient’s individual preferences.
Julie Gregory: And I thought, I’m sorry Dale, I’ve got a quick question. Do you ever use a patch? I hear you’re talking about cream but what about patches?
Dr. Hathaway: Absolutely. I have, you know, at least 50% of my patients use a transdermal patch. It’s a very good method. It gives a very stable level, you know especially for people who, for whatever reason, their level tends to bounce around a lot. You can get some people who will trend toward getting hot flashes. And if you even on the hormones and so a patch will typically work better for them. And some people like the convenience of just having to put a patch on twice a week. So yeah, a patch is bioidentical estradiol and it’s very effective and it’s very convenient.
Dr. Bredesen: And then Donna is asking also is prometrium a natural progesterone.
Dr. Hathaway: Yes, it is. That is the, you know original commercially available through regular pharmacies trade name for oral micronized progesterone, and oral micronized just means that it’s better absorbed right from the intestinal tract. And that is a, very good source of progesterone. The only issue with prometrium, and now there’s some other, but the same thing in generic form. But the only issue with that is that it only comes in two doses, 100 milligrams or 200 milligrams. And for some women that’s not the right dose, right? Some women need 75, some women need 250. So, but for me prometrium is a very good product and works very well.
Dr. Bredesen: And I know you’ve recommended this in the past a lot for people as they’re going to bed, it also helps you sleep and that you can take it orally 100 or 200 milligrams. And so is that usually the way you start people out with a nighttime dose of a 100 or 200 orally?
Dr. Hathaway: Yes. That would be a very common way that I would start someone out. It definitely many many women are amazed at how much it helps with sleep. It doesn’t help everyone, but it’s quite common for sleep to improve on progesterone at that kind of a dose. So, you know, if you’re putting them on a fairly hefty dose of estradiol, you would trend towards starting with the higher dose of progesterone around 200. If you’re starting with a lower dose of estrogen you would probably start with the dose closer to 100.
Dr. Bredesen: And do you cycle the progesterone or not?
Dr. Hathaway: Yeah, it’s very individual, you know, theoretically the best way to use progesterone is to cycle it. Two weeks and two weeks off or three weeks and one week off. The reason why that’s theoretically the best is that that mimics our normal female physiology where we produce progesterone, for half of our cycle before menopause, right? When you cycle and it’s thought that, the progesterone receptors, are more sensitive this way and react more appropriately. Right? So many times I start women out on 21 or 24 days of progesterone per month. But the problem is some women will have withdrawal bleeds on that, every month and of course that’s not something that post-menopausal women wanna put up with. Some women will say, my goodness I sleep so well, every day when I take the progesterone but then every time I stop it, my sleep is terrible. So then I will switch them and I’ll keep them on it continuously. You have to watch the dose. You don’t want the progesterone to be too high or too low. So I do follow that, but you know, there’s pros and cons to each side of that cycle or continuous progesterone question.
Dr. Bredesen: And do you find that people tend to do better with their cognition when they’re just on the estradiol without the progesterone? Or do they tend to do just as well when they’re on both?
Dr. Hathaway: Yeah. I haven’t seen a significant difference, in terms of that, no, I mean, there are some women who are intolerant of progesterone and that’s a whole other topic. It’s kind of a longish one, but oral progesterone, when it’s metabolized, it metabolizes into something called allopregnanolone related to pregnanolone , but different. And that, is what makes you tired at night. And that allopregnanolone binds to a kind of receptor called GABA. A GABA receptor in the brain which is our most sedating. GABA’s our most sedating neuro-transmitter, right? It’s good. You know, we, it helps us be calm and it helps us sleep. But some women respond negatively to this excess GABA stimulation and they can get depressed. So you’ll get, I’ll get women calling me saying, I can’t stop crying, there’s nothing wrong in my life, I don’t know what’s going on. But this progesterone is just, you know, bad for me. Or you’ll get people who are sedated all day, no matter how low a dose you give them or you’ll get people who are irritable, you know very irritable on progesterone. And there’s a lot of Scandinavian literature on this, and what the Scandinavians write, is that if you give it as a vaginal suppository, progesterone vaginal suppository, you can avoid this, the all these negative GABA related effects. And I found that to be true, in about 80% of women I can avoid those negative issues, if we switch them to a Avastin spot story.
Dr. Bredesen: And then also the dose. So when you initiate the estradiol, what dose do you typically start with?
Dr. Hathaway: So it depends on, where the woman is in her post-menopausal life. If she’s newly post-menopausal, I would typically start with a 0.05 patch in a smaller woman and a 0.075 patched in a little bit larger woman because, you know, weight matters, you know, and so, that would be my starting dose. And then I would see, you know, what their level was as I said, I’d like to see a woman early in menopause at a level of at least 50 on up into, you know the 80 to 100 range, depending on how she reacts. If a woman is, certainly if I’m starting a woman in her 70s, I’m gonna start on the lowest dose of the patch. If she’s been off as, I mean sometimes you run into a woman in her 70s and she’s only been off estrogen for a year or two. You know, someone finally decided to take her up in which case I’m much less you know concerned about starting her at hereto, a 0.05 patch, but usually I will start someone who’s been off estrogen for more than 10 years. I would start them with a 0.05 patch because you’re more likely to run into a side effect temporary side effect, like breast tenderness, which often can be resolved by taking iodine by the way, the breasts really needs iodine to be healthy.
Dr. Bredesen: Great. All right. And then Karen says here that sail through menopause at 48 and not even one hot flash didn’t have any problems. Didn’t look into replacement hormones for that reason but then found out about being four four and started bio-identical at 65. Was that too late? And it sounds like from what you’re saying it’s still a good idea for Karen as a four four to be on a BHRT.
Dr. Hathway: Absolutely. She would wanna make sure she’s on a topical estradiol. She would wanna get her, estradioll, hopefully up to 50 at least, make sure she’s taking progesterone with that and has a good level of progesterone like for a level of estrogen of 50, I like to see a blood level of progesterone of at least 3.5, if not 4.5 to five.
Dr. Bredesen: Okay. And Julie, obviously this is exactly the sort of thing that you have dealt with, with so many people unable that info. So what do you recommend for someone who’s 65 who is equal to four, four, and starting VHRT. What other things should this person be thinking about?
Julie Gregory: You know, we don’t make recommendations obviously, and in our community, women share their stories. But one thing that comes up over and over again, is that we’ve noticed a lot of thin women have a hard time getting their estrogen levels up. Have you noticed that, Ann? because I take the highest dose patch, 0.1 milligrams and you know, it gets me to like 40 or 50. So, you know. I was just wondering if that’s a phenomenon there too. If you noticed.
Dr. Hathaway: To some degree, but it’s more variable than that at least in my experience, thinner women especially women who are very fit, one thing they have is they will run a higher SHBG, Sex Hormone Binding Globulin, which binds the estrogen and carries it around the body, along with a few other proteins that carry it around. And when you have a high SHBG, you may need a higher free estrogen level. You mean that need to get to a higher, because some it might be harder to get to a higher free estrogen level because so much is bound to that, SHBG protein. I have so many people in my practice who, because I’m very fortunate to have a very, you know, healthy group of people who tend to come to me, they almost always run an SHBG that’s above normal. So that could be one reason why, you know thinner women may need to be many to have a higher dose than you would expect for their size.
Dr. Bredesen: And will come back to the fact that, we were talking about someone who’s an ApoE4/4there are about 7 million Americans who are four four. And as we’ve talked about before, the chance of developing Alzheimer’s during your lifetime if you are a four four is very high, well over 50%. So please, if you’re completely asymptomatic at least to get on PreCODE if you have any symptoms whatsoever consider getting on ReCODE, because there is a tremendous amount you can do and we can really make it so that people who are able four positive do not have to worry about this problem. Let’s cut the number of people in this country with dementia as far down as we can.
Dr. Hathaway: One thing that the, a sub study of another big study showed was that women who carry the ApoE4 gene when they’re on hormone replacement their telomere shortening is very significantly reduced. Right? You saw, I’m sure that study Julie, very, very very interesting study. So even if you’re not symptomatic, you are still having telomere shortening which eventually is going to have a negative impact.
Julie Gregory: Yeah. Our community is very pro bioidentical for months. And I know you’ve probably visited our site (apoe4info.com) before Ann but we have a thread devoted to that. That’s probably 200 pages long so I mean it’s very fabulous.
Dr. Hathaway: Overwhelming. Overwhelming. Yeah. Fantastic.
Dr. Bredesen: Yeah. I mean, the reality is, you know this should be a very, very rare problem, cognitive decline if people do the right things. And especially if you get the notification that you are able to be for positive. Absolutely please get on optimal prevention or reversal as soon as possible. So then one of the other important things that Deborah brings this up here, how do you find a good doctor? And so if you’re out there somewhere, how do you find the appropriate doctor who is knowledgeable about BHRT?
Dr. Hathaway: Yeah. I’m, that is something where one does need to do a good research. I would, of course, look at, at your gynecologist in your area and think about who among those gynecologists is not practicing OB and might be a little more aware and up-to-date on menopause, because a lot of gynecologist if they do OB that is an overwhelmingly compelling area of their practice, and I recently talked to my new gynecologist because my old one retired and she told me she had had one leak in her four years of training on menopause and then she proceeded to pump me with questions for about an hour after that, she said we are completely inadequate in our educational menopause. So if you, you know, I would search for somebody who advertises that they’re aware and have developed a practice that includes BHRT. So that would be one suggestion. If you look at the providers on Apollo, you’ll find that, you know many of those people are educated in BHRT. There’s other resources but you do have to do your research because as I’ve mentioned many times, there are many many gynecologists out there who are still recommending that women are doing well on their hormones, stop them at age 63 or 65. And that is absolutely, a very uneducated, unfortunately, an uneducated opinion.
Dr. Bredesen: And if someone is going to stop them, do you recommend that they cold turkey them or you recommend that they dribble them down slowly?
Dr. Hathaway: I would taper for sure. Yeah.
Dr. Bredesen: And next question here from Susie, who says I take sublingual progesterone with a topical estrogen and testosterone. My mother recently began getting pellet shots every three months, which delivery system is most effective.
Dr. Hathaway: I’m not a fan of pellets. There are practitioners who swear by them and some patients who like that, but once you have those pellets in it’s very difficult to adjust the dosage and removal of those pellets is, it’s gruesome actually to get those out. So, because we can do so well with the kind of delivery systems we have that don’t involve, you know injecting things, injecting foreign bodies into your skin. I strongly prefer avoiding pellets. Some people like it and promote it because they say that’s the only way you can get the high levels. But I think we have good, like, we now have good techniques when you include the vaginal delivery to get very, very good levels and in any women who we put our mind to it.
Dr. Bredesen: Yeah. And then Karen is asking is a five-day break advised using bioidenticals post-menopause. So do you have a break in there or do you continue the hormones throughout?
Dr. Hathaway: Yeah, I continue estrogen in my patients, all the time throughout the month, as we mentioned earlier for some people a break in progesterone is recommended and some women do very well with a five-to-10-day break, five even to 15-day break in their progesterone.
Dr. Bredesen: Yeah. And Donna is saying here taking Premarin vaginally to prevent chronic UTI. I’ve had a breast biopsy back in 2000 removed atypical hyperplasia and a fibroid Now, what to do to prevent cognitive issues. Now, obviously already on Premarin as opposed to estradiol what do you recommend to Donna?
Dr. Hathaway: So a very, what she’s most likely using is a very very low concentration of Premarin cream. So she’s not very unlikely that she’s getting any significant systemic estrogen production, right. But again, it is effective for genital urinary syndrome or atrial fib vaginitis. The two names that we refer to it by, but it’s not going to be giving her the cognitive benefits that you want to have with estrogen. So, you know, I would recommend that she see someone who is, who has expertise in BHRT and get herself on a good regimen with good levels of estrogen and progesterone.
Dr. Bredesen: Okay. Then Sally’s asking how about prescription she’s on the protocol and she’s got a prescription for some progesterone is in the form of a capsule. Does that mean it’s real or not? Well, as you’ve pointed out that you actually to contain bioidentical orally so that shouldn’t be a problem, obviously it depends on what the prescription is. It just says for progesterone. So yeah, please, we would recommend please make sure that it is bioidentical. And then let’s see here, Wendy mentioned what do you recommend for maximum levels of hormones?
Dr. Hathaway: So generally, for estradiol 100, I will say I do have two patients who absolutely insist that their estradiol level be over 200. That that’s the only way they feel well, and I do maintain them with precautions at levels of about 200 to 250. And those are not crazy levels of estrogen when we are cycling premenopausal women’s estradiol tends to cycle through the, through that regular menstrual cycle from anywhere around 70 or 80 in some women all the way up to 400 in other women. Right. And you do go through a period where you’re very low rate at the time of your menses and right after that, and then your estrogen gradually builds up and tends to peak right around the time of ovulation. And then it goes down a little bit and then there’s usually a little hump up a little bit and then it drops again. So during that time, when it’s at its peak in some women it’s only at 180 or so in other women, it’s up at 400. So we do have a big range and a big variation of what’s biologically normal for estradiol levels. So it’s quite possible that these women really do better. And what we absolutely really need is some really good research that really tells us what levels do what in the brains, in the hearts and the bones of of all of our post-menopausal women and hopefully the tide is gradually gradually turning as I’m sure. I know I’ve mentioned this to you several times Dale and Julie you probably know this as well that at the December 2019 Breast Cancer Symposium, the biggest most important Breast Cancer Meeting in the country, the San Antonio Breast Cancer Symposium. The headline of the conference was estrogen lowers breast cancer risk. And this is by, this presentation was given by Chleblowski the head writer for the WHI Women’s Health Initiative study which of course scared all women out of using hormones. My generation, for the most part they all missed the benefits of hormones, because of that 2002 report that came out. And I don’t wanna overstate the case because with estradiol alone, there was a decrease in breast cancer and a decrease in death from breast cancer of 44%. But when you added to the Premarin, the synthetic progestin and there was a slight increase in breast cancer. So I don’t know about you, but for me that strongly suggests that that synthetic progestin, Medroxyprogesterone is the culprit here. And we know that that synthetic progestin is, has multiple Daryl deleterious effects. I mean, on bone, on heart, on, on everything. There’s no reason of course, why. And very few gynecologists if anyone is using that anymore, thankfully. But this whole idea that, you know hormones increase breast cancer risk. It’s so deeply embedded in our culture almost. It’s almost like, it’s hard for anyone to believe that that’s not true, that at least if you’re taking hormones, you are taking a risk, in terms of breast cancer. And, you know, I think the evidence in the tide is turning strongly that if you’re using bioidentical estrogen and real progesterone, it’s very very possible that there is absolutely no increased risk and possibly a decreased risk of breast cancer.
Dr. Bredesen: Great. So I’d like to squeeze in just a couple more here. If we could, Donna asked me this is very relevant to what you just said. She’s Donna says she had a mastectomy 23 years ago was told never to use estrogen. She’s now 64. It sounds like the suggestion would be find it up-to-date expert to address readdress this at this point. And then Jena asks, what would you recommend for a 44-year-old woman in perimenopause who has a mother with early Alzheimer’s diagnosed at age 63?
Dr. Hathaway: So, she’s 44. She’s in perimenopause, she’s in a perfect place to seek out an expert and start herself on a topical bioidentical estrogen, either a patch, a gel. There’s a commercially available gel called estrogel. That’s been available in France the same product since the 70s. So, and make sure that she gets on a bioidentical progesterone as well. But if she’s having symptoms of perimenopause absolutely it’s time to seek out the right expert and get started on her hormone therapy.
Dr. Bredesen: All right. Thank you so much. Thank you, Anne. Thank you, Julie. And please everyone stay safe. We’ll take the rest of the questions online and again, everyone. Thanks very much for excellent question. So please stay safe and let’s prevent and reverse cognitive decline. Thanks.
Dr. Hathaway: Thank you.
Dr. Bredesen: Thank you. Thanks again.




