April 26, 2021
Facebook Live: Special Considerations for ApoE4 Carriers – Parts 1 & 2
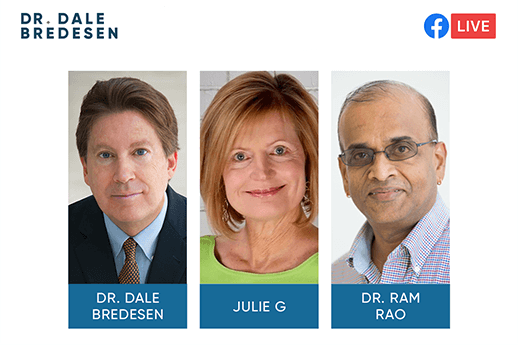
Apollo Health’s Chief Science Officer, Dr. Dale Bredesen; Chief Health Liaison, Julie Gregory; and Principal Research Scientist, Dr. Ram Rao, discuss the ramifications of ApoE4 and the special considerations carriers need to take to prevent neurodegeneration. Drs. Bredesen and Rao took a deep dive into the ApoE4 protein and how it acts as a “master control” affecting 1,700 genes, while Julie Gregory shared her insights into how this science translates into clinical practice. Topics covered include: why ApoE4 carriers have a greater need for ketosis, the importance of avoiding insulin resistance, protecting your head from injury, and more. For your convenience we have included the full transcript of part one below the video.
Watch part one:
Transcript Part One:
Dr. Bredesen: Hi, everybody. I hope everybody is staying safe and hope everybody’s doing well and welcome to Julie Gregory and Dr. Rao. We’re so happy to have you both here today.
Julie Gregory: Thank you. Happy Friday.
Dr. Bredesen: Happy Friday.
Dr. Rao: Yup. Thank you so much. It’s a pleasure.
Dr. Bredesen: So perhaps the most important question that comes up repeatedly is, what is it about ApoE4 that makes things different? and why is this the most common genetic risk factor? So, if you look at all the people who have Alzheimer’s disease, about two thirds of them are ApoE4 positive. Also, as we’ve discussed before, if you look at the likelihood of getting it throughout your life, here’s the way it breaks down. So, if you are APOE4 negative, so you’re a three three or a two three or a two two for example and that’s about three quarters of our population. So, about 230 or so million Americans you do have a lifetime risk of about 9%. It’s not zero, but in certainly we do see especially with the toxic variety that it’s type three. We do see this, but if you are APOE4 positive if you have a single copy, you associate you’ve gotten it from one parent or another. And that is about 75 million Americans. It’s about 25% of the population or so, then your lifetime risk for Alzheimer’s is right around 30%. Now there are all sorts of things that affect that. And as Julie knows better than anyone, you can drive that down to virtually zero by doing the right things. And that is the era we are now entering where the Alzheimer’s is becoming an option. It’s not becoming ineluctable. You can prevent yourself and you can especially early on, get a clear reversal. On the other hand, if you have two copies and that’s about 7 million Americans it’s about 2% of the population. Then your lifetime risk is well over 50% in some studies approaching 90%. So, it’s more likely that you will develop Alzheimer’s some time during your life, then you will avoid it. And so, therefore we would like for everybody we should all be finding this out. And again, the old-fashioned notion was nobody find this out because there’s nothing you can do about it. So, just forget it.
Dr. Bredesen: And of course, when the human genome was sequenced, the human genome was sequenced from the original one from James Watson, who said, I don’t want to know my status because there’s nothing, I can do about it. And again, that’s completely changed. There’s a tremendous amount. And so we encourage everybody. Please find out your APOE status, because if you are at high risk, there is a tremendous amount you can do. And that’s what we be talking today. And then in one follow-up and condition about what to do about this. So, let’s talk a little bit about the background. What’s really interesting. One a why is it that this one gene out of your 20,000, so 22,000 or so genes this one protein that is produced is so common and so incredibly important in risk for Alzheimer’s. And I should mention if you go back throughout history the earliest hominids back between five and 7 million years ago were all ApoE4 96% of our evolution as hominids, we were all four fours just in the last 220,000 years, APOE3 appeared. And then in about the last 80,000 years APOE2 appeared. So, these are relatively recent additions to the human genome. And what’s really turned out is that ApoE4 has a pro-inflammatory effect, and you can ask, well why would you want a pro-inflammatory effect? But it turns out actually to be quite important if you’re walking around on the Savannah and you’re stepping on dumb and you’re getting infections and you’re eating raw meat this was all pre fire back then, you’re eating raw meat, that’s full of microbes. You need that pro-inflammatory effect to survive. And this was first suggested by Dr. Tuck Bench represented down at USC. And I think Tuck was absolutely right about that. But for years it has been unclear about how the heck this thing which is acting like your butcher. It’s the thing that carries around some fats. What the heck would that have to do with Alzheimer’s disease? And, I may be a little biased, but I think the most important work on that question has been done by Dr. Rao, who’s with us today and Ram and I and our laboratory colleagues started a project years ago to ask that very question, why is it that having ApoE4 is such an important risk factor? What are the molecular mechanisms and Ram determined something very exciting which is that ApoE4 actually, doesn’t just bind to a receptor and go inside your cell. It actually goes into the nucleus. And so, Ram, maybe you could talk a little bit what did you find that actually explains so much about what ApoE4 does, but it’s actually not just your butcher carrying around the fats it’s also your Senator, it’s making the laws of the land. It’s actually changing the programming of your cells.
Dr. Rao: Yeah. So, I mean data just as you put it so well, you know it was never taught that ApoE4 could do this because as you said rightly pointed out, our ancestors had this gene. And in fact, that was a dominant gene and they needed that. They needed that because, you know, when they were going out in the open, they live for, I mean, you know they had to hunt, they had to, you know, walk on the grass. So. they were actually grounded between which we are now enforcing it in our practice here. So, they were grounded. But then in that process of grounding, you know they were getting not a bruises. They were getting wounds, they’re getting infected. And what did ApoE4 do to them? It protected them. It actually prevented them from getting a massive ear infection, or inflammatory state because ApoE4 was there to protect them. But now fast forward and we are in a hyper competitive world. We are in a stressful world. We are living in a century lifestyle and our food is all got changed. We are no longer eating the kind of food that our ancestors were eating. And so, what happens now that same ApoE4 this is a term that aging scientists like to call the antagonistic pleiotropy the same gene that was very helpful. Now over time in your, in your lifetime it becomes a sort of detrimental to our health. And so, you know, one of the big questions was this is the one of the main risk factors for Alzheimer’s disease. And the question was, what was it doing? I mean, there were a lot of people who worked on it. We were not the first ones people work before us. But what happened is those are the times when the amyloid story and the tau phosphorylation story where you know, sort of the babies in the osmosis field. And so, everyone was rushing in to put their theory that you know, sort of merge very well with either the amyloid theory or with the Tau theory. And so, you know, when we searched the work did. I mean, you and I talked about that. We said, you know, could they be some other mechanism? And because we were in the aging field the first thing we noticed was, that it actually, there was some interaction of ApoE4 with a gene called SIRT1. And SIRT1 1 as we know, is what we call the longevity gene. It promotes longevity and it has got so many other protective functions. And what we showed is that, in place of ApoE4, SIRT1 1 actually gets depressed, which means, and SIRT1 also has a role in Alzheimer’s because SIRT1 1 actually plays a role in activating one of the enzymes that is involved in cleaving the amyloid precursor protein into a direction where it provides protection to the system, no synopsis, synaptic formation and laying down all the synaptic capacity network and all that. SIRT1 1 was helpful in that way. But now, because ApoE4 was present, SIRT1 1 got repressed which means all the good effects of amyloid precursor protein, was no longer present. And so, the question we asked is this. And this was fascinating because we were the first ones to show that actually interacts with the longevity gene. But what was interesting was Dale, we also showed that the interaction was not at the protein level, but it was at the DNA level, which means that you know SIRT1 1 and ApoE4 had, there was something about the DNA protein interaction that causes the SIRT1 1 to go down. And so, you know, as you mentioned correctly people in the lab like Huygens and Alex and other people, they started looking at it more closely and sure enough they found out that ApoE4 was not a passive guy, ApoE4, actually you know, it was acting like a transcription factor. That’s a mouthful for people who not the scientist but what it means is that, it regulates a lot of other genes downstream. In addition to SIRT1, ApoE4 was regulating so many other genes. And what we showed is, and, you know they were so excited when we saw that …
Dr. Bredesen: Yeah.
Dr. Rao: the results, those genes most of them are all involved with Alzheimer’s disease. Whether it was genes for inflammation, whether is genes for longevity, whether it’s for cholesterol levels estrogen regulation, neurotoxicity, snaps formations. All the genes are regulated by ApoE4. So, you know, that opened up big as sort of a Pandora’s box where we showed that ApoE4. So it’s not like a one time or a one small reaction ApoE4 does, so many … things in the cell.
Dr. Bredesen: Right, It’s a master control gene. Yeah.
Dr. Rao: Absolutely.
Dr. Bredesen: Now let’s translate what you found in the lab which I think is an absolutely beautiful finding into what this means for us as human beings who are trying to keep our cognition and trying to avoid or reverse cognitive decline. And so it’s interesting what you found and Ram found that 1700 different genes are affected by ApoE4. Just amazing. And that includes, as you said, SIRT1 1 critical it includes things that are related to inflammation, includes things that related to hormonal regulation. It includes things that are related to glucose metabolism. It’s just an amazing, amazing gene. So here’s the bottom line. We’ve talked about the fact that what Alzheimer’s really is at its fundamental nature is an insufficiency in support of a neural network for plasticity. So you can get your on the making and keeping. So you’re either in growth mode or you’re in protective mode and you’re pulling back with protective mode. This is just what happened with COVID-19 protective mode. We’re pulling back, we enter a recession. So, what ApoE4 does is it makes you more protective it’s as if you had a city where they would call the police at the drop of a hat. So, it is a more protective mode and therefore there’s more of the protection and pulling back then there is the growing forward. And it’s important to emphasize there It’s not better to be able to be ApoE3 or ApoE4. They’re different. They each have advantages. They each have disadvantages. The good news is if you know what you are then you can live accordingly. And actually, I think Julie has some tremendous insights into what works best. So Julie, let’s just start with what sorts of things in terms of nice, before I get there, I should say, you look at third world countries, the Quechuan Indians in Bolivia the Ghanaian in Africa, these people live longer. If they are and do better, if they are ApoE4 positive because they need that protective mode.
Dr. Rao: Hm.
Dr. Bredesen: On the other hand, as you indicated Ram, if you’re in a society where it’s not about protection you’re not getting ongoing pathogens and inflammation and parasites every day you actually then live a little bit longer as an ApoE3. But again, if you do the right things you can balance them both. So Julie, let’s maybe start with ketosis, talk a little bit about metabolism and ApoE4 and how do you recommend the people who find out their APOE status and find out their ApoE4 positive who should not worry they should feel fine. And actually, we know you’re going to do a great job and live for a long time let’s make sure to optimize things for you. So let’s talk a little bit about ketosis.
Julie Gregory: Right? So I think what we’re burning is that ApoE4 carriers have a greater need for ketosis. We have lot’s and lots of evidence that at a very early age as early as the beginning of the third decade. So 20-year-olds, when they do brain imaging or having a reduced ability to use glucose in the brain is fuel.
Dr. Bredesen: Yeah.
Julie Gregory: And what’s very interesting is that when you study the patterns it is the same regions of the brain as Alzheimer’s patients.
Dr. Bredesen: Right.
Julie Gregory: but yet you’re seeing this reduction in asymptomatic young adults.
Dr. Bredesen: Yeah.
Julie Gregory: So, the good news is, we can replace that neural fuel deficit with ketones. And, you know, that confuses some people because I think it’s well known that ApoE4 carriers don’t do a good job with a lot of dietary fat. We tend to hyper absorb dietary fat. So when people hear ketosis, they automatically think we’re recommending butter and bacon and we’re really recommending a lifestyle protocol. So for me, as an ApoE4 homozygote, I fast for an extended period every day, at least 18 hours, sometimes more took me a long time to build up to this, but I feel amazing doing this. And by fasting, I’m naturally creating a mild level of ketosis. I’m also very physically active. I exercise for an hour or two every day a couple of dedicated sessions but in between that I’m active as well. I look for opportunities to move throughout the day and you’ll notice that the way I’m describing the lifestyle I’m describing is very similar to how our primitive ancestors lived.
Dr. Bredesen: Yeah.
Julie Gregory: They didn’t eat three meals a day …
Dr. Bredesen: Right.
Julie Gregory: and they didn’t snack in between, and they were constantly moving and exercising. So I’m taking a cue from them …
Dr. Bredesen: Right.
Julie Gregory: and I’m mimicking that applying it to this modern lifestyle. And it’s a very simple way to get a mild level of ketosis. Of course I avoid sugar and any refined carbohydrates I eat a lot of non-grain plants. Also lots of wild caught seafood, some limited grass fed meat and lots of healthy fat. So, I worry less about macronutrients ratios when you’re applying those other two strategies. When you’re already in ketosis from a long, daily, fast and exercise.
Dr. Bredesen: Right.
Julie Gregory: Dietary fat isn’t as important.
Dr. Bredesen: Now, what do you recommend for people who are very thin and say I just can’t fast but I’d still like to get my ketones up because I recognize you know, this is, again, this is about an insufficiency. This is a chronic insufficiency supporting your brain. Just as you said, you look at a pet scan you can see the reduction in glucose utilization even in the twenties. And so we recommend people get started early get those ketones up so that you can have the combination and you can have that ability to switch the metabolic flexibility to switch between the glucose and the ketones. And I know in your case you do a lot of polyunsaturates and monounsaturates so that you don’t have the problem with saturated fats. So, what do you recommend for people who are thin and simply don’t want to do the fasting?
Julie Gregory: Well, I think there comes a point when you can be too thin because they’re all lots of thin people. I think my BMI is around 19 and I do very well with the long daily fast, but when the BMI begins to slip below 19 and you get into 18 and even lower, I think a long daily fast can be a bad idea.
Dr. Bredesen: Yeah.
Julie Gregory: So, what you can do is you can eat still eat less often but eat very high-quality food. And of course avoid sugar starchy carbs and emphasize the healthy fats, you know things that the brain needs.
Dr. Bredesen: Okay. Now, I know Mary Newport has written books about getting people exogenous ketones. And I know that in the past before you were doing full exogenous or endogenous ketosis you used to occasionally take a little just a small amount of MCT. And what do you recommend for people there? Do you ha do you recommend MCT oil, coconut oil? Do you recommend ketone salts or esters? What sorts of things?
Julie Gregory: Right. So for first of all, if you’re insulin resistant it’s very difficult to fast for extended periods. So. you need to do this slowly and extend the fast by a few minutes every day. But, at the time that I was insulin resistant I wish I would have known more about exogenous ketones. I think that can be very helpful in that instance, I think for ApoE4 carriers, it might be the ketone salts and esters that are the most helpful because we do tend to have this exaggerated response to saturated fats that are in coconut oil that are in MCT oil.
Dr. Bredesen: Right.
Julie Gregory: And some people may say, high cholesterol is not a problem. It is a problem when the person is also insulin resistant, it’s a very bad combination to have the elevated cholesterol. So I think the ketone salts and esters are a great idea.
Dr. Bredesen: Yeah, that’s a very good point. And certainly one of the points made in the past is that ApoE4 there’s this increased risk in cardiovascular disease which is not present for those who are insulin sensitive. It’s only seems to be for the ones who are insulin resistant. So, that brings us to the second point, which is let’s talk a little bit about insulin resistance. There are something like 80 million Americans. So, before you get type two diabetes you have a quarter pre-diabetes but before you get pre-diabetes you typically have a pre pre-diabetes which is essentially insulin resistance. And again, you can go back, right back to the molecular basis of this where you can actually measure the changes in your insulin signaling.
Dr. Rao: Yes.
Dr. Bredesen: and see that you are signaling molecules, something called IRS1 which is downstream from your insulin receptor is actually physically changed with specific phosphorylation groups. So it’s really saying, I’m recognizing there’s been too much sugar and too much insulin and therefore I’m going to turn things down. And unfortunately, you now have a system that’s not responding as well as it should. You are developing insulin resistance, which is associated with increased risk for cognitive decline. So, Julie, how do you combat insulin resistance?
Julie Gregory: Well, it’s interesting when I was insulin resistant, I didn’t know that I was, and my physicians didn’t tell me that I was. It wasn’t something that they were looking for back then. This is nine years ago. I was having hypoglycemia throughout the day where I would almost lose consciousness and I couldn’t figure out what was going on. And my physicians were telling me to eat more starchy complex carbohydrates; I wasn’t eating enough. So, it creates this vicious cycle.
Dr. Bredesen: Yeah.
Julie Gregory: given by mainstream medicine I would say avoiding insulin resistance is the most important strategy for ApoE4 carriers hands down. And how do you do that? By using the lifestyle strategies that I just described by using a long daily fast by exercising and by eating a low carbohydrate diet that’s primarily whole foods, non-brand diet.
Dr. Bredesen: Yeah. So here’s a simple way for people to find `out if they have insulin resistance, very simple take a look at your fasting glucose. You should be below 90. We’d like to see, you know, seventies, eighties. That’s great. If you’re now getting 90, a hundred, 110 you’re starting to get too high of a glucose. But before that happened your body tries to pour out extra insulin. So you multiply your fasting glucose. Let’s say your fasting glucose is 80. And let’s say your fasting insulin is five. So, 80 times five is 400. And then you divide that by four or 5.45. That’s the number that gives you that will convert it to what’s called a HOMA-IR.
Dr. Bredesen: It tells you whether you have insulin resistance. And if that number, if that ratio is greater than 1.1 you’re on your way to insulin resistance. As it’s getting up to 1.5 and two. So people we run into, for example who will have fasting insulins of 10 and fasting glucose of 90, well, the doctor will say, well your glucose is okay, but wait a minute glucose times that times the 10, you know, 900. So you’re now, well all over two for your HOMA-IR. So you really already have fasting. You already have an insulin resistance state. So, this is the good thing, because it will tell you it gives you a warning before you ever get to type two diabetes. So, easy to do to take your numbers or ask your practitioner. And you can find out what your HOMA-IRs. And if, again, if it’s over 1.1 you’re heading towards some insulin resistance. So, please be careful and think seriously about getting on more of an insulin sensitizing approach just as Julie has outlined. And then of course there’s been a lot about how the brain heals itself whether it be from head injury, whether it be from stroke whether it be from other insults, like insulin resistance like pathogens and all these things. And so, Julie, what do you recommend for people who are interested in football or interested or are concerned about riding motorcycles or getting who or who’ve gotten into car wrecks and things like that, auto accidents, what do you recommend to them?
Julie Gregory: I think you make a compelling point for people learning their APOE (status) as early as possible.
Dr. Bredesen: Yes.
Julie Gregory: I wish I could have. When I have grandchildren, I hope to encourage my son and daughter-in-law to have their children’s APOE status checked very early on because my son is in ApoE4 carrier and he engaged in lots of dangerous sports that I would not have encouraged had I known his APOE status. So, first of all, know your status, second avoid sports like football, anything where you can have impact— boxing, when you do ride a bike or go on a motorcycle or go skidding, wear a helmet. It’s very simple. I learned that the hard way when I recently had a brain concussion. I was skiing and I was taken out by a couple of snowboarders and I hit my head really hard on the way down. In a car wear a seatbelt. I mean, protect your head.
Dr. Bredesen: Yeah.
Julie Gregory: and just use common sense. But first of all, know your APOE status.
Dr. Bredesen: Great point …
Dr. Rao: On that note Dale So, you know, just so that people don’t get the wrong impression that ApoE4 carriers should not be doing any physical activity or should not be engaged in sports. There are a lot of be engaged in sport because there are now lots of studies to show that ApoE4 carriers actually higher physical activity is associated with greater cognitive functions. And it’s interesting because if you link it with the beta-amyloid which is of course the baby for everybody, you know in those people who engage in physical activity not only do they have improved cognitive function I’m talking about the APOE carriers, but they also have low levels of beta-amyloid. So, and these benefits actually are less pronounced in ApoE3 and ApoE2. So ApoE4 do very well when they do physical activity they actually do very well. But of course, as Julie mentioned, you know if you’re engaging in physical activity make sure that you take proper precautions.
Dr. Bredesen: Yeah. That’s such a good point because it really does say if you are ApoE4 positive, great you actually are going to do better with exercise. You should absolutely be doing exercise it’s quite important. And so absolutely believing that, that’s a certainly a good thing to remember. And we should add in general people who have done the recode protocol we’ve gotten good results with people who are ApoE4 positive and negative. But in fact, the ApoE4 positives tend to get even a bigger response than the ones who are ApoE4 negative. I think in part, because the ApoE4 negatives are often the type three, the toxic ones but for whatever reason, the ApoE4 tend to respond very very well. So, I think that’s a very, very good point.
Dr. Rao: And you know, that’s true because even among the you know, just like the way, you know we have the ReCODE program that we have out there and then the PreCODE program in the same way, you know we had this huge study that came out from Finland they call it the finger study.
Dr. Bredesen: Yes.
Dr. Rao: or the Finland geriatric intervention (FINGER) study.
Dr. Bredesen: Right.
Dr. Rao: They talk about it. And, you know, they use similar protocols that we use You know they have diet exercise, that mental training vascular risk factors, they try to address all this. And guess what? Dale, Julie also knows about this. When they subdivided their population, they notice that the ApoE4 carriers actually did extremely well in all these interventions. They seem to have responded much better, much faster. And the amplitude of the positive response was even quicker compared to the E3s and the E4s.
Dr. Bredesen: Yes. So That’s a good point. And then as Julie said, sometimes you can’t avoid it. So, you know skateboarder knocks you over or something happens. So, okay. We’ll make sure to be on appropriate prevention. If you are ApoE4 positive and you have had a head injury please be on things like whole coffee, fruit extract things that are going to increase your BDNF get your hormones, optimized, get your nutrition, optimized minimize your inflammation, all these sorts of things that can help you for many, many years to come. So, this has been a fantastic background. Let’s go to some questions. We’ve got some wonderful questions coming through here. So, let’s start here. We have one from Lori. So, Lori says I’m a four (ApoE4) four from Southern California. And again, there are about 7 million Americans who are four fours and the vast majority don’t know it. I would hope that everybody would find out and make sure that this becomes a rare disease. Let’s make it so that we prevent it in everyone’s ApoE4 positive. And for those of us who were ApoE4 negative as well. So, she says, I’m looking forward to lifestyle recommendations. I currently have intermittent fasting. So, she’s doing 16, eight, very much like a Julie. Fantastic. And of course, Julie has a wonderful website that she started “ApoE4.info”, tremendous information for anyone who is interested in ApoE4 and cognition focus on eating mono fats and veggies low animal protein also would love thoughts on COVID. So, Julie, let’s throw these two to you here. First of all, low animal protein. Now I know you’ve written about this actually in the last book the end of Alzheimer’s program, you wrote a lot about that about macro ratios and about how much protein. I know you are a fish eater especially and pastured chicken and things like that. What do you recommend as far as animal protein?
Julie Gregory: Well, I think what we like to recommend is about 0.8 to 1.0 gram per kilogram of lean body mass. So, there’s many exceptions to that for people that are over age 65, for people that have gut issues especially those taking peep PPIs and have reduced the acid you know higher amounts are necessary.
Dr. Bredesen: Well, what about people healing …
Julie Gregory: Yeah.
Dr. Bredesen: people have CIRS and are dealing with these sorts of immune issues, often need more, people who are healing from various things. So yeah, all these.
Julie Gregory: But it’s, that’s not a draconian restriction by any means.
Dr. Bredesen: Yeah.
Julie Gregory: And the only restriction that we put on there is for animal protein; we are never restricting vegetables as all plants have some protein. So, for a woman who is about 130 pounds that ends up being about two small, pastured eggs and a piece of salmon, that’s about 4.85 ounces a day is within those restrictions. So, it’s not draconian by any means.
Dr. Bredesen: Absolutely.
Julie Gregory: Yeah. It’s important your body cannot produce protein. We need to get, take that in. It will cannibalize your muscles if you don’t get enough.
Dr. Bredesen: Right. Yeah. And people will say, well. Hey, I want to be a vegetarian. That’s fine. No problem. You can be a vegetarian; you know you could be a pescatarian. You, you can do this anyway. The bottom line is to get the appropriate things to prevent and reverse trying to decline. Now let’s talk a little bit about COVID-19. This is an issue of course, for everyone right now, there are people who are very much set against vaccines. People who are very much on the vaccine side. And so, and a no question with ApoE4 as with so many other things, what stroke outcomes of head injury outcomes, the outcome in on average for people who are ApoE4 positive is worse than it is for people who are ApoE4 negative. Now what’s interesting. They didn’t do the other half of the study and I’d be very interested there. My guess, just because you have a more pro-inflammatory state which is why the outcome before you have more of a cytokine storm, my guess is, you are probably a little more resistant to getting it to begin with.
Dr. Bredesen: but once you get it, it may be worse. And so, for sure, all of that’s been found about limiting the cytokine storm using things like montelukast and using things like dexamethasone things that will calm that cytokine storm are going to be more important than ever with people who are ApoE4 positive. But so, you are able, and for Julie, what have you done about COVID-19? Yeah. This may not be perfect for everybody but for yourself.
Julie Gregory: I also wanted to mention that study that you referenced only looked at a population of people that were hospitalized.
Dr. Bredesen: Yeah, exactly. That’s what I’m saying.
Julie Gregory: We are not hearing about ApoE4 carriers who developed COVID you know and didn’t develop severe symptoms. So, I think the risk factors that affect everyone of course affect us as well. So again, avoiding insulin resistance, you know and I’m taking some specific supplements right now that I wasn’t taking before. I’m doing the AHCC that you recommended.
Dr. Bredesen: Yeah.
Julie Gregory: and maintaining social distancing and all that kind of stuff. But I’m still outside exercising outside every single day. You know …
Dr. Bredesen: Yeah.
Julie Gregory: all that upregulates our immune systems. Spending time outdoors.
Dr. Bredesen: Absolutely. Yeah. Again, you know, neither one is better or worse. It’s slightly different. You’ve gone toward more. You are more, I say a hair trigger. You’re going to jump into protection mode quicker. And that can be a very good thing when it comes to gut parasites. And it can be a very good thing when it comes to pathogens. And in many ways, on the other hand you have to be careful in the long run. If you’re exposed to too many inflammagens germs you may have this overreaction which over time could hurt you. But again, since we can see this coming for many years ahead of time, there is so much we can do again. Alzheimer’s should be a very rare disease. Okay. So now, Catherine asks any recommendations for resources to learn more about extended fasting? Julie, do you have favorite resources for extended fast and Ram, do you have favorite resources for fasting?
Dr. Rao: Well, I mean, I don’t have any resource, there are so many out there. My only worry is that Dale the ones that I’ve seen it’s too much on the fasting thing, you know? So, the ones that I’ve seen at least, they fast for three days continuously and binge for the entire day. And then they come again, the fast for, so that’s in my opinion, that’s too much. It’s good to maintain 15 to 18 hours of fasting, but anything beyond that, especially if you have sick health conditions, I would not go gaga or those prolonged periods of fasting. I mean in both in our practices via our notice account, anywhere from 14 to 18 hours offer regular daily practice of fasting is really good. And keeps you in that mode where you can starve off you know, I’m, noticing even though this is not been there’s no study out here, but all those people that I know of, who have been on an overnight fast for 14 to 18 hours at least the one I didn’t carry out the study, but all those people, Dale and Julie they’re all so far touch wood. They have not had any infection from the COVID. So, I’m not sure if it’s a fasting, but definitely, you know fasting combined with other things. But definitely there’s, you know the 14-to-18-hour window is really good.
Dr. Bredesen: Yeah. And Julie, what about you?
Julie Gregory: I think Dr. Jason Fung has some good information on fasting and I also would invite Catherine to join “apoe4.info”. It’s a community created for ApoE4 carriers and we talk extensively about fasting there.
Dr. Bredesen: Yeah. I think that’s a great point. And you, of course, Ram you’ve written a book and you included a discussion of fasting in your book. And of course, same with you, Julie you’ve written in the end of Alzheimer’s program about fasting and that’s again important. And I think it is important. You know, all things in moderation. We’re not suggesting that people try to go for a week without food. Now, if you have some extra pounds. And in fact, we used to do this when I was a resident at work, people who had significant type two diabetes would be brought in with a controlled fast and it would really help their type two diabetes. But if you have no extra fat to burn and you are going to go an extended fasting you can actually hurt yourself. And there are some recent articles. Actually, I had brought this up recently this study that showed that you can actually over the long haul, have some degree of heart damage. If you’re going on these extended, extended fast with no fat to burn. So, please be careful what Ram and Julie’s saying is absolutely correct. That I think that, you know, 16 hours, 18 hours. Great. So if you have a time window just as we’ve heard earlier here from Laurie, time window where you’re eating for eight hours or you can even make that four hours fine but you don’t want to go long, long long periods unless you are trying to burn fat and you’ve got fat to burn. So, let’s see here. Karen asks, what would a typical exogenous ketone supplementation look like for someone? How much, how often? Great point. So, some people like to use more of an MCT oil where you’ve been used in workups slowly. You could use up to a tablespoon three or four times a day here please be careful of your LDL particle number.
Dr. Rao: Yes.
Dr. Bredesen: If you will be saying, you’ve been hurt your cholesterol. You can hurt your lipid numbers. And so many people who are ApoE4 just say, I want to stay away from the MCT oil and the coconut oil because they are saturated fats. Okay, no problem. Then you want to use ketone salts and esters. And one of the ones that I’ve tried myself which I happen to like is called KE1. It is a mixture of salts and esters which is a nice combination. And again, you want to work up slowly. You take the whole little bottle which is about six CCs. It’s about two ounces and you’re going to go, Whoa! it really opened up your eyes. So, I started at literally a quarter of that and then try that once a day and then work up slowly to where you’re doing the most you want to do is to a little bottle, two ounces three times a day that will bump your levels. And you’ll notice it when you take this because you get kind of a fairly immediate rush like, wow, Hey, things are exciting. It’s a little bit like that. You know, you’re really someone throwing water in your face or something, you know, like, wow, I’m awake. Okay. But again, in the long run, the best is for endogenous ketosis generating into cells.
Dr. Rao: Yes.
Dr. Bredesen: But in the short run, you can use this to get things going because it does help your brain. And we find this again and again and again people who are getting into ketosis to tend to do better with prevention and reversal of cognitive decline. All right, let’s go to the next one. So Tim says as a child with what eventually became known as an illness related to many increase in a diet high’s salicylic acid foods. I was put on a special low salicylates diet banned from even a baby aspirin. Okay. All this was forgotten, and I was on daily, low dose Bayer. Then we had micro bleeds. Okay. Very good point. Microbleeds are often associated with males who are ApoE4/4. So I always tell people if you’re a male and it turns out you’re four four, especially if there’s a family history of cerebral hemorrhage or hemorrhagic stroke, please get checked out. There’s an MRI that you should do, which is called MP RAGE, where you can look specifically for any of these microbleeds. You wanna get on top of that because you wanna basically then make sure that your vessels are peyton but you’re not shutting things down which is what causes this amyloid to form in them and ultimately can potentially bleed. So you wanna get better flow and you wanna stay off things that thin your blood too much. You don’t wanna have a lot of Omega 3s for example, if you’ve got these little microbleeds. So very good point about these and there they are relatively common especially in four four males. And then here Mel asks. So just to clarify, if you’re not insulin resistant and you’re ApoE4, MCT or coconut oil? Good. Well, here’s the thing. Check to see what your LDL particle number if you’re still running in the 800 to 1200. No problem. If you’re sitting up there at 1800, 2000 that’s gonna be too high. And actually Julie was the one who first suggested you know, get yourself moving over from the saturated to the more of the monounsaturates and the polyunsaturates. You’re still getting the advantage of the fats without the disadvantage of those. So, what do you recommend Julie, for people who are ApoE4 positive and, but they’re not insulin resistant in terms of getting their ketones up?
Julie Gregory: You know, everyone’s different, as you said she could start with MCT or coconut oil. If she is insulin resistant and unable to endogenously create ketones. But the ultimate goal is to let your body naturally create them with this long extended fast with exercise and a low carb diet. And when you put the three together, it’s really very easy. I mean, you don’t need to do any of those to any extreme measure.
Dr. Bredesen: Yeah.
Julie Gregory: So, I’d be, that’s the ideal way to create ketosis.
Dr. Bredesen: Absolutely. The next one Laurie is saying, the formula again for HOMA-IR. So good point. And we should all know just like there, all these things you know, we should all know what our fasting insulin is. We should all know what our HS-CRP is. We should all know our APOE status. So HOMA-IR if you wanna do is take your fasting glucose and you wanna multiply that times, your fasting insulin. And so again, a good one would be, you know, fasting glucose of 80 fasting, insulin of five, that gives you 400. You wanted them divide that by 405. That’s all you need. You don’t need to worry about the 0.4 or five. It’s kind of irrelevant. 405. So you’re at 400 divided 405. You’re just under one. You’re essentially at 1.0, that’s where you wanna be or even a little lower than one. It’s when you’re getting up above 1.1. So here’s another example. You have someone who’s got a fasting glucose of a hundred, and they’ve, which is fairly common. Unfortunately, you’ve got a fasting insulin of 10 you’re working overtime just to keep that hundred. So, that’s 10 times a hundred cents a thousand. Now you’re going to divide that by 405. So, you can see you’re over two already. So, you are quite insulin resistant at two. And as you get up at three, that is high that we have insulin resistant. We see this all the time where people will have HOMA-IR of four or five, six, eight, you know very high from the combination of a high insulin. Now what happens where this starts to lose it is when you’re starting to lose your ability to make that insulin. So, now that people have been you simply can’t make any more. Now you’re headed for diabetes. So, that’s why you wanna know ahead of time. It’s telling you, are you already insulin resistant and on your way, we’ve got a deal with it now, otherwise, what will ultimately happen is your pancreas will start losing the ability to make that insulin. And now your hemoglobin A1C is going to go up and your fasting glucose as we go. And now you’re getting type two diabetes.
Julie Gregory: Hmm.
Dr. Bredesen: Okay. The next one is from Andrea who says I’m really struggling with finding information about ApoE2,4 combination? That’s a good point. And if you’re two four your intermediate, it’s less than a three four in terms of your risk for Alzheimer’s but it’s more than a three three, for example. So, you’re in between there. Most studies show three or four heterozygous and homozygous not considering three two. Yes. three two is the least common. It’s the most recent it’s the one that appeared 80,000 years ago. So some say as long as there’s one for you might as well have both but this doesn’t make any sense. No, absolutely. You’re right. Having one four is not the same thing as having two fours. It’s a difference between about a 30% risk of lifetime versus well, over 50% because it is different. And a two-for is a little bit less than a three, four so you’re below 30, but you’re above nine. So you’re in there in between somewhere. So good idea to follow the things that the APOE four carriers are following. And Julie, what about, how do you deal with this on your website with the apoe4info? Cause I’m sure you’ll have many, two fours.
Julie Gregory: Yeah. I don’t know that we have many, but this is a discussion that has come up many times.
Dr. Bredesen: Yeah.
Julie Gregory: And there’s some things that the E2 allele and E4 have in common. E2s do poorly with a lot of carbohydrates. So, and they tend to get very high triglycerides. So, the diet that we generally recommend for is perfectly suited for E2,4.
Dr. Bredesen: Great point. Yeah. And certainly, grain is a big issue for many of us for many of us in the United States and all over the world. But especially as you said, for ApoE4 and especially for those who are getting high triglyceride levels. And so again …
Julie Gregory: Yes.
Dr. Bredesen: here’s another good thing to know check your triglyceride to HDL ratio. It should also be right around 1.0 as you’re getting above 1.3, your triglyceride to HDL you’re getting that two and three. That is increasing your risk for cerebrovascular and cardiovascular events. So, good to know your type.
Julie Gregory: I was just going to mention it’s the ApoE2s that are susceptible to the carbs. So, they have an exaggerated response with high triglycerides.
Dr. Bredesen: Yeah. when they make … Good point. And then the next one here is from Diana, who says can you clean your APOE status from the data collected in 23 and Me genetic testing. And I absolutely. And I know Julie, that’s where you started. So maybe you mentioned a little bit about that.
Julie Gregory: Right? You know, I’m not sure how they’re reporting it now. I think if you have ApoE4 you are notified about that but I think currently they’re otherwise not telling you your status, but you can run the raw genetic information through a program called “promethease.com” and you can figure out the information that way.
Dr. Bredesen: Couple of years ago, they would, if you remember they were the FDA had them take it off but then they put it back on. So, now you have their five genes that they will allow you to look at and APOE is one of them. So, actually you should be able to clean this. I haven’t checked in the last weeks, but absolutely. You should be able to get it from there. You may have to.
Julie Gregory: Yeah. You can tell if you’re ApoE4, but I think if you’re not ApoE4 they don’t provide the information and they’re constantly changing that. So that, that could have changed.
Dr. Bredesen: Get your point.
Julie Gregory: But the raw data … Yeah. You can still figure it out.
Dr. Bredesen: Got it. Okay. And then let’s see here, Kathy says so interesting. My husband is an ApoE3,3 and again, that’s the most common one and is toxic. Yeah. And this is the problem with the three threes and the two threes tend to be the ones who get more type three toxic cognitive decline. They are less on the other types of cognitive decline that ApoE4s are more susceptible to. He says what was a natural athlete should you continue exercising? Absolutely. Exercise is important for all of us. They ApoE4 positive, ApoE4 negative. Doesn’t matter. It turns out to be very, very helpful for all of us. And again, and Julie wrote very nicely about this in the book, both for some strength training which helps you, especially with your insulin resistance and for cardiovascular training, very helpful for your ketones very helpful for a cerebral blood flow. Very helpful for your oxygenation, all of these things. So, both of them very, very helpful. And then Carrie asks, any particular diet recommendations for high TSH levels, but medium, low thyroid? Yeah. Very, very good point. And TSH TSH is going up again. You are struggling.
Dr. Rao: Exactly.
Dr. Bredesen: It’s just like having insulin resistance. You’re struggling. You’re putting out extra TSH to make your, to whip your body and to shape the producing that. So, you wanna find out if it’s because you are deficient in iodine or not. If it’s an iodine issue, you wanna have more kelp you wanna have more exposure to ion. If it’s not an iodine shooting what certainly wanna find out if you have antibodies, you may have some Hashimoto’s thyroiditis. So, which is very common and often associated with leaky gut. So yes, you need to get checked out a couple more tests to see please talk to your practitioner about what’s causing this high TSH level. And I know there’s a nice newsletter from (Dr.) Izabella Wentz. Who’s been through a Hashimoto’s herself and talks about the many things that are related to this and has some very good tips about how to deal with this. Let’s see the next one is Sean. Many of us diligently follow the end of Alzheimer’s protocol daily, fast and carb high model and saturates daily ketosis. Finding that our fasting blood sugar is creeping up over time. Some argue it’s a phenomenon called physiological insulin resistance and can be ignored but it results in a poor homa-IR, please help us understand what’s happening and how to proceed? Julie, you talked a little bit about this in the book. I don’t know if you wanna say a few words about this kind of creeping up of the glucose that is sometimes seen over time.
Julie Gregory: You know, that might be a sign that it’s a good idea to do periodic carb feasting.
Dr. Bredesen: Yeah.
Julie Gregory: And that doesn’t mean unhealthy carbs. It still means the carbs that we recommend but maybe one day a week or so eat more carbohydrates. And another thing to look at is look at your HbA1c. Cause we see some people that do have that high fasting glucose, but the HbA1c which is a check of your blood glucose over three months if that’s still well below 5.3, chances are this is not a significant issue.
Dr. Bredesen: Yeah, that’s a good point. So, the hemoglobin A1c gives you an integrated look of what your glucose is doing over a couple of months. So, that’s a good thing to look at. If it is creeping up, then it’s a good point. I think that going through some, you know going through some cycles some people will liberalize once per week. I mentioned how people, again, to be more sensitive on the next one Ogi asks, and I make only for homozygous in Africa my parents never had any issues, such a good point. And again, this goes back to when you’re doing all the other things appropriately. This is the ancestral gene. And you know, when it appeared five to 7 million years ago of course it did appear in Africa and this was not a problem. And this was not a problem for people still in this day who are living in in certain sort of situations. It is more of a problem as Julie often points out that our ancestral approach is not the same as our modern approach. So, to some extent, this is a problem that is brought on by the way we are living today. And we do have to go back to more of that ancestral understanding as Julie said earlier, getting up more moving, you know, less grain, less processed foods. And this is certainly important. Now Ogi says I’m 37. I have severe bad memory. Okay. So please get on an appropriate protocol. So, is after a spinal cord injury from epidural and have not recovered. Okay. From, I assume you mean an epidural hematoma from the injury insulin resistance. Okay. Can’t do the intermittent fasting. I get very dizzy. So, how do I go about intermittent fasting? Okay, so good point. So, what you can do find out you may wanna start with some exogenous ketones and to help you start slowly, get you start get getting to your intermittent fasting slowly. And this is a common thing that people will have problems at the beginning. And then of course also again Julie has written about the Keto flu. Many people have issues at the very beginning that partly related to loss of electrolytes as you’re kind of as you’re dumping this, this glycogen. So I would, I would start that way. Julie, how do you recommend people getting into intermittent fasting when they’re just starting out?
Julie Gregory: You know, I was the same way with hypoglycemia so I can totally relate.
Dr. Bredesen: Yeah. And this is the appropriate time for CGM, as you said.
Julie Gregory: Beautiful.
Dr. Bredesen: So finding your glucose monitor because you can see a lot of people the problem is they’re spiking and then they’re going into a trough. And so then you wanna have more fat and you may need some more protein to smooth that curve out so that you’re not going up. So many people are surprised when they do CGM. So Ram, let me just ask you, what do you recommend in Ir? You are an Ayurvedic physician trained and practicing. What do you recommend for people with Ir to do you check with people who come to you? Do you check their ApoE4 status and what do you recommend?
Dr. Rao: No, we don’t check their ApoE4 status Dale. But what we do is if there’s ApoE4 or ApoE2 we put them all on abroad intervention. Intervention is with regard to the fasting stage. I tell everybody irrespective of their ApoE4 status because you know, some of them, they may not even have the ApoE4, you know, for direct consultancy. We don’t to look at that. But it’s very interesting because in Ireland what we say is there are three ways to develop they didn’t call it ketones. They didn’t call it ketosis. But they said along with fasting what you can do to improve your cognition that’s what they specifically said. And they said, before you break your fast go ahead and indulge in at least 30 minutes to 45 minutes of physical exercise.
Dr. Bredesen: Mmm-Hm.
Dr. Rao: And then they said after that, before the physical exercise, they said, engage yourself in a 30 minutes, mental training or brain exercise. Okay. And then after the brain exercise was done, then they said indulgent 30 to 45 minutes of physical exercise. And then you break your fast. Now, if you go back and look at these three events, they may seem independent but now we know all two of them, they have one common pack that they convert into the BDNF pathway. Okay. And then that it’s all the same factor. But down downstream is the same pathway. Finally, leading to ketone production, ketone bodies.
Dr. Bredesen: Yeah.
Dr. Rao: So, that’s where I tell them, I say, okay 12 hours of 12 to 13 hours of fast. And then one hour of physical exercise and the mental exercise. I tell them to either learn a language or learn a new skill or learn a new instrument or try to, you know memorize some lyrics of a song or something. And then after that, I’ll tell them to move 30 to 45 minutes of either yoga or walk or run gym or whatever they can. And then, you know, by the time it’s like, when they finish off all that, it’s nine, nine 30 in the morning. Perfect time for them to have breakfast.
Dr. Bredesen: Yeah. Great point. All right. Thank you so much, Julie. Thank you, Ram, for the excellent discussion. Thank you everyone for the great questions. We’ll take the rest of the questions and answer these online. And again, thanks everyone. Let’s make it so that no one has to worry about cognitive decline. This is the goal for all of us. So, thanks very much.
Dr. Rao: All right.
Dr. Bredesen: See you next time. Thanks so much. Bye everybody. Bye Julie.
Julie Gregory: Bye bye.
Part two of the Facebook Live session, continued with additional considerations for ApoE4 carriers, including a discussion about alcohol usage, how dietary fats affect lipids, the controversial role of grains, the potential need for higher amounts of omega-3s — including which groups need to exercise caution with fish oil supplements and much more. For your convenience we have included the full transcript for part two below the video
Watch part two:
Transcript Part Two:
Dr. Bredesen: Welcome everyone, I hope everyone is continuing to stay safe and healthy. Great to be here today with Julie and Ram. Welcome, Julie, welcome Ram.
Julie Gregory and Ram Rao: Thank you.
Dr. Bredesen: And we want to continue, two weeks ago we talked about special considerations for people who are APOE4 positive. And to put that into perspective there are 75 million Americans who have a single copy of APOE4. If you have zero copies, which is about three quarters of the population, then your chance of developing Alzheimer’s over your lifetime, somewhere around 9%. It’s not zero, but it’s not terribly high. If you have a single copy, it’s about 30%, and again, that means 70% chance you won’t develop Alzheimer’s, but it does put you at increased risk. And if you have two copies, then it’s well over 50% and more likely that you will develop it, therefore we suggest that everyone, please check your status. It used to be said, don’t check your status because there’s nothing you could do, actually, there is a tremendous amount you can do. And of course, Julie founded a site ApoE4.info where thousands of people share their information and share optimal procedures for improving their cognition. And of course, preventing cognitive decline and reversing cognitive decline just as we published a number of years ago. So I think there’s a tremendous amount that can be done and everyone should know their status and should get on appropriate prevention. I wanted to just start by mentioning that Dr. Rao Ram who’s here with us today has done some really exciting basic research to understand how it is that APOE4 actually gives you this increased risk. And what he found was actually quite surprising. What he found is that the APOE4 itself, the molecule, which carries fat, so would’ve been thought of as kind of like your butcher, it’s the guy who carries some fat around, everybody thought that this thing was just a carrying fat and doing nothing else. And what Ram found was really surprising, when it binds to receptors on your cells, it actually enters the cell and then surprisingly a part of it, not all of them but some of the molecules go into your nucleus. So what we thought of as your butcher carrying around the fat is also your senator making the laws of the land, changing the programming of your cells. So, Ram, could you talk a little bit about the fact that you found 1700 different genes? So this is a remarkable control, it’s really changing the fundamental mode of your cell to more of a pro-inflammatory more of a pro-protective sort of mode. And in fact, you see that if you go to the third world people who are APOE4 positive do better, they do better with things like the various parasites and things like that. On the other hand, you do have this increase in inflammation. So Ram, if you could just mention a couple of these 1700 genes that you found that APOE4 does actually, it actually comes and sits on the promoter, so the upstream region of these genes and it pushes them down, including things like SIRT1 as you first described several years ago.
Dr. Rao: Right, yeah and that was very interesting because by then people had already known that ApoE4 is one of the biggest risk factors. And they also said that when you have ApoE4 especially if you have two copies, then you are at a greater risk. But the question is, nobody knew what exactly happens when you have the two copies of ApoE4. How does that translate to having more AD or Alzheimer’s disease? And the problem was those days, people were looking at A-beta story and they’re looking at the tau story because these are the two prominent theories then going around and so people are looking at ApoE4 versus A-Beta and ApoE4 was this tau. And then around the same time, as we all know there were people coming out with drug discovery campaigns and drugs for A-beta tau were just not working. And so then we took this project, we tried to see whether there is something more than what it is, more than the A-beta or the tau story. And sure enough what we found is, and this is amazing finding that we had because we were in an aging institution and so the question was can relate this to some kind of an aging theory. And sure enough, what we did is, one of the first molecules that we noticed that was playing a role in this, if you bring in the A-beta and the tau theory, is a gene called Sirtuin 1 or SRT1. And SRT1 is concept to be the longevity gene, people have reported that you have SRT1, you live a long life, you are protected from so many age-associated conditions. And what we showed actually, when I did this beautiful work what it showed us that ApoE4 you actually suppresses or down-regulates the SRT1 activity. So imagine now you have a protective molecule, SRT1, and now that protective molecule is suppressed, when you have ApoE4 present on that. And so now that it’s suppressed, all things happen, we notice that there’s more of A-beta levels going up, tau phosphorylation is going up, all because the SRT1 levels have come down. Now, the question was, is it affecting at the protein level? Well, you know, we did a lot of experiments and we just couldn’t find a protein-protein interaction and so it seemed as if there was something else happening. And, I casually mentioned to him, I said “Maybe it’s acting at the DNA level.” That was surprising because nobody had reported that APOE4 can enter the nucleus and bind to the DNA, but that’s what happened. We showed that it enters the nucleus and it binds to nearly 1700 promoter sequences of so many different genes. And what we did we segregated all these genes into their function properties and sure enough nearly a hundred or more than a hundred of these genes appeared to be involved in some capacity in Alzheimer’s disease. SAT1 was definitely one of the candidate genes that we showed, including in addition to SAT1, we also showed a lot of other genes that are involved in inflammation, estrogen levels, in diabetes insulin signaling pathway, apoptosis, and then in a signal transduction mechanisms, synaptic plasticity, neurotransmitter binding. So it seemed as if a lot of the genes that are involved and which had some role to play in AD, ApoE4 seems to be, at least in some of the genes that we noticed, it was suppressing the activity of all these genes. And what was interesting was most of the inflammatory genes that APOE4 was down regulating, it seemed as if it was favoring more of the inflammation part and down-regulate the trophic support path. So trophic support was down neglected, inflammation was going up. And that may very well explain as to why we have so much of toxicity associated with inflammation and withdrawal of trophic support. In addition to that, Dale, we also notice one more thing. One of the theories is that there’s hyperphosphorylation of tau, right? And so we were looking at what is causing that. And again, another great finding from our genetic studies and from our protein binding studies, one of the proteins that is involved in hyperphosphorylation of tau is a phosphatase, right? And this phosphatase actually removes the phosphorylated molecules. So that what happens is tau becomes a normal protein tau. But what happens is when you have APOE4, it actually suppresses this activity on this phosphatase protein. And because it suppresses the phosphatase, you now have more of phosphorylation of the tau and once you have more phosphorylation this hyperphosphorylated tau is now causing all the disassembly of the microtubules. So everything that we wanted to explain in terms of neuroinflammation could very well now be a part of what ApoE4 was doing in the sense that suppressing all these genes that are so-called protective genes and thereby amplifying the entire informative responses.
Dr. Bredesen: Right, so let’s talk about the practical implications, I think that’s a key issue here. So what we found over the years in the laboratory is that there are these two modes going back to what is really, what is Alzheimer’s at its most fundamental nature. It is an insufficiency of a network that you require to make and keep synopsis. And so just as we saw this with COVID-19, what happens in COVID-19 we’ve gone from more of a growth mode for our country to more of a pulling back in a protective mode. That’s the same thing that your brain is doing when you have all these insults, whether it’s because of too little oxygenation, when you’re sleeping or metabolic syndrome, inflammation, poor food, toxins ongoing stress, in any of those situations, your brain is moving from a mode of growth and making and keeping synopsis to a protective mode. And what you found with APOE4 very interesting, is that it pushes you more toward that protective downsizing mode. So it’s more important than ever to avoid these various insults that are causing you to go into that protective mode. So let’s talk about some specifics now. Julie, I know you’ve been living this for a number of years now, talk about a little bit about what are the implications of being APOE4 positive in terms of handling alcohol? Is this something that you should be aware of? Is this something that people should consider and should be changing based on their APOE4 status?
Julie Gregory: Yeah, it’s important to look at the totality of evidence. So when you look at alcohol consumption, a small amount seems to be protective for cardiovascular disease and for dementia. So we see this U shaped curve, we see people who completely avoid alcohol, they’re actually at higher risk for dementia and then on the other side, we see people who drink heavily, are at much higher risk for dementia. However, when you stratify all of the research by APOE status, ApoE4 carriers tend to do worse with even a little bit of alcohol. And that’s kind of hard for a lot of people to swallow. It’s important to understand that this research has been done with datasets of people who aren’t living the neuroprotective lifestyle, that many of us are, who are probably insulin resistant and using the standard American diet. And for that reason, if you do consider using alcohol we certainly recommend a very small amount. We like dry red wine; I use less than four ounces. We like red wine because of the health benefits, and I use it from Dry Farms Wine. So, it’s low alcohol, it’s no sugar, it’s organic. And you know, I occasionally have a little bit, but it’s a tough thing for a lot of ApoE4 carriers especially when you find out at a young age.
Dr. Bredesen: So certainly in moderation and certainly the Dry Farms brand is one good way to go. Let’s next about the absorption of fatty acids. When this comes up commonly, we often recommend to people if you’re APOE4 negative, go ahead and do 12 to 14 hours of fasting at night. If you’re APOE4 positive, think more about 14 to 16 or even more than 16. And I know you yourself, Julie, do something more like 18 or 20 hours of fasting, you have a time restricted eating of about what four to six hours.
Julie Gregory: I do, I do, and I think this does help with the hyperabsorption of fatty acids. I’d like to think that I’m living more ancestrally. We know ApoE4 is the ancestral allele, and so certainly our ancestors were not eating three meals a day plus snacks in between, which really tends to get us in trouble with our lipids. Another thing that we recommend for ApoE4 carriers is to consider minimizing saturated fat and prioritizing the poly and monounsaturated fats. And we’re talking about fats from primarily whole food sources like from avocados, nuts, seeds, fatty fish, cold pressed high polyphenol extra virgin olive oil. In the ApoE4 community when we see people make that shift away from saturated fats, their lipids tend to be much better.
Jday plus snacks in between, which really tends to get us in trouble with our lipids. Another thing that we recommend for APOE4 carriers is to consider minimizing saturated fat and prioritizing the poly and monounsaturated fats. And we’re talking about fats from primarily whole food sources like from avocados, nuts, seeds, fatty fish, cold pressed high polyphenol extra virgin olive oil. In the APOE4 community when we see people make that shift away from saturated fats, their lipids tend to be much better.
Dr. Bredesen: Yeah, it’s a very good point and I think, and Ram you want to talk about–
Dr. Rao: Yeah, definitely.
Dr. Bredesen: In relation to APOE4?
Dr. Rao: Yeah, there’s this interesting study Dale, Julie I don’t know if you’re also there, but so this is, I mean, he calls it the right gene, the wrong environment. This is a guy from Arizona State and he wanted to understand what exactly happens with ApoE4 when you compare in our ancestors and you compare the present day age. And so what it was, and he calls it two different societies he calls it the industrialized society APOE4 and then he calls it the tropical environment E4. And he went to this Amazon Forest where you have this tribe, the Tsimane tribe.
Dr. Rao: Tsimane Indians.
Dr. Bredesen: In relation to APOE4?
Dr. Rao: Yeah, the Tsimane Indians and what he noticed was these are the people who live in groups in the forest and to communicate, they happy to walk for miles or they have to use the trees and the lower hanging branches to jump from one to another just to meet the other people. No sanitation, proper sanitation, no running water, no electricity and remote population, always exposed to parasites and pathogens. So if you’re concerned that type 3, these are the right kind of people who will have the type 3 kind of disease because they are always exposed to pathogens and parasites. And on top of that, most of them have APOE4. But what’s interesting was what he noticed is that these are the people, who, and you know, even though are tribal people he did cognitive tests on them and what he noticed was they did amazingly well on all the cognitive tests, they did so well. And despite being exposed to parasites or the pathogens, their brains were absolutely perfect. I mean, they didn’t have any issues of memory losses, they’re very good in some of the skills that they had and they were, it seemed as if the ApoE4 had absolutely no role to play in their health, at least in their environment. So that’s what he says when Julie talks about the grains, he says, so Timbal says the same thing he says, if you were to adopt that kind of an environment here probably the E4s will do much better. You may not have the cognitive kind of complaints that you normally have in terms of whether it’s fat digestion or whether there’s any other situations.
Dr. Bredesen: Yeah, I think it’s so important to point out because when people find their genetic status they often would feel worried about it. And I know people will say, “Oh my gosh, I found out “I’m ApoE4 positive and I’m, this is horrible.” No, it’s not horrible and in fact, you’re 75 million Americans, and in fact none of them should get Alzheimer’s. The reality is this should be a rare disease. So we don’t want to scare people by saying please check your status. Because in fact, there’s a tremendous amount you can do and knowledge truly is power and it’s its power to change your life and make your life longer and more productive and keep you sharp until you’re a hundred, which everyone should be. And I think it’s important also to point out a number of people have asked about, what about APOE4 versus APP presenilin-1 and presenilin-2 and what they call familial Alzheimer’s disease. So that’s a very important distinction, and here’s the way this works, for 95% of people who get Alzheimer’s disease that is sporadic Alzheimer’s. In other words, it’s not necessarily in the family, it’s not as specific mutation. Yes, APOE4 increases your risk, but it is not your fate. And again, as Julie and thousands of others have pointed out and have shown beautifully with their own stories, it is not your fate. So this is just a tremendous amount you can do about it. Now in just the 5%, one out of every 20 people, there is a specific mutation, and it can be in one of three genes, APP itself which is rare, presenilin-1, presenilin-2. And now in that case, the people who get the mutations typically do go on to get it, it’s pretty much 100%. And we are working with some of these people now to see if we can drop that because there are hundreds and hundreds of families worldwide who have, for example these various mutations, for example, APP. And I do think that now that we understand better and better what these are actually driving, we will be able. We want to start with people who have those mutations even in their twenties, because they will often get the disease in their thirties or forties, often very young or fifties. So please, if you are aware that you are a part of a family with PS-1, PS-2 or APP, please get on prevention even earlier to do the best we can. There may be additional things that need to be added because that is different than a risk gene, that is a, in the past, at least that is a certainty gene. So that’s the fundamental difference. There’s a tremendous amount that we know that we can do with ApoE4. So we’ve talked about fats a little bit, talk a little bit about ketosis, if you would, Julie, where do you stand? And do you think it’s best to do essentially metabolic flexibility where you’re going in and out of ketosis or do you think it’s better to keep ketosis for a long period of time or is either one acceptable?
Julie Gregory: I think it depends where you are in your journey. I’m metabolically flexible and I move in and out of ketosis throughout the day. And I’m primarily ketotic through my very long, extended, fast as opposed to eating lots of fat because we know what happens when ApoE4 carriers do eat a lot of dietary fat. So I live ancestrally. I loved that you shared the story of this Amazon tribe Ram, because they not only have low risk of dementia, they have very low rates of cardiovascular disease by living primitively and by eating a hunter gatherer type diet. I really try to live a more primitive ancestral lifestyle. I think when you’re insulin resistant, getting back to your question, Dale, it’s important to get into ketosis however you can. Because when you’re insulin resistant, your brain is being deprived of fuel, so at that point we have a crisis. And so whether you use exogenous ketones or you can endogenously get into ketosis through combining exercise, fast and diet, we want you to be in ketosis to give your brain the fuel it needs but once you’ve healed the insulin resistance I think the goal then shifts to achieving metabolic flexibility.
Dr. Bredesen: Yeah, that’s a very good point. Okay, and then talk a little bit about ApoE4 and grain-based diets.
Julie Gregory: Right, so this goes back to what Ram was talking about. Some people have proposed that this is a great example of the mismatch theory. We know that the APOE4 gene is the ancestral gene. For millennia, we ate non-grain plants and we hunted animals and ate fish that we caught. We ate whatever we could get our hands on but we were not eating grain. Grain is a new kid on the block, it’s only been around for about 10,000 years. So some have proposed that ApoE4 carriers will do better by abstaining from grains. And there’s many, many reasons to consider that. One, we know that the standard American diet is very high in processed grains, which leads to insulin resistance. So that right there is a wonderful reason to avoid it. We also know that grains in the United States are very different from grains anywhere else in the world. We’ve hybridized our grains to the point where we produce very profitable crops but they’re also very damaging to us in terms of causing inflammation— widespread inflammation throughout the body, but also to the gut. And our use of specific chemicals like glyphosate just exacerbates that. And then there’s the work of Dr. Alessio Fasano, who’s found that gluten, which is found in wheat, rye and barley leads to a permeable or leaky gut not only in people with celiac disease but also in those with non-celiac gluten sensitivity, and maybe everybody. So when you’re eating gluten, you have this leaky gut which is particularly bad for APOE4 carriers because we already have a leaky blood-brain barrier. And the theory is that toxins are escaping from the gut and getting into the brain.
Dr. Bredesen: And so we’ve got a couple of questions coming through here several questions coming through, but before we get there, let’s quickly address two final things. One is the Omega-3 change and the potential change in homeostasis for Omega-3s, does that suggest a change, should people who have APOE4, should they be eating more on the fish side and less on the actual supplementation side for Omega-3s? Should they take altered supplements, or they should, should they take standard supplementation? I know you’ve often recommended they should make sure to have an Omega-3 index at least of 10 or above, so what do you recommend? And I certainly think everybody should know their Omega-6 to omega-3 ratio and/or their omega-3 index. So what do you recommend there?
Julie Gregory: The research is mixed because some research shows that ApoE4 carriers benefit from supplementation, some shows we don’t, the methods are all different. Sometimes they check omega-3 index before and after supplementation, sometimes they don’t. But what’s interesting is that when you look at omega-3 in the periphery and in the central nervous system after any amount of supplementation, ApoE4 carriers have lower levels. So to me, that kind of sends a signal that we either need more, or we need a different kind. And I know you’re aware of Dr. Rhonda Patrick’s theory that ApoE4 carriers should be getting their Omega-3s from fish, from fish roe or from krill oil. She thinks the phospholipid form of DHA may be most effective for us.
Dr. Bredesen: Yeah, good point.
Julie Gregory: Right, but I just want to mention something. It’s important to understand that when you look at an all ApoE4 data set, those that have the highest omega-3 indexes have better brain function and structure when you compare to those with the lowest levels. So that tells me that it’s very important for us to pay attention to this and definitely check omega-3 status. And I get mine above 10 by eating seafood and fish. I also supplement with DHA and I’m taking the plasmalogen precursor which is another form of Omega-3, so I feel like I’m hopefully covering my omega-3 status through a number of different bases.
Dr. Bredesen: Yeah, and certainly more and more are interested in plasmalogens and their relationship to cognition. And let’s just finish before we go on to the questions here with the issue for those people who are males who are ApoE4/4, who have two copies. They do have an increased risk for having amyloid within the vessels. This is called congophilic angiopathy or amyloid angiopathy. And when this invests itself in the vessels, there are actually two things that happen. Number one, the vessels can actually leak, you can get some bleeding. So you want to be careful about having a large, what’s called a lobar hemorrhage because it’s out in the lobes of the brain. And the other thing is that, so you want to be careful about taking a lot of omega-3s. You don’t want to have a lot of blood thinners and just ask your doctor, please check my MRI to make sure I don’t have micro hemorrhages. If you’ve got these micro hemorrhages, that’s a concern especially if you are an APOE4/4 male. The other issue though, is it can also cut off the vessels so that you now have reduced supply. So you also want to do exercise and some people like to do things like EWOT, exercise with oxygen therapy. You want to have exercise; you want to keep those vessels open. You want to keep the blood flow, you want to keep the oxygenation. There’s some suggestion that part of this bleeding is because you’re not getting enough support, so you’re now creating a situation very much the way you see with macular degeneration. You’re now getting new vessels, which can potentially bleed. So please check with your physician, if you are a 4/4 male, especially if there is a family history of hemorrhagic stroke, please talk to your physician. And meanwhile, let’s now run to the questions here, there’s some excellent questions here. Christine’s asking about the book too, little F words about time restricted eating. Yes, great point, it’s got some recipes, no refined sugar, gluten free. That’s fantastic and actually Julie is now going to be putting out a book that’s about the appropriate things for the KetoFLEX 12/3 Diet. I’m very excited about that and I should mention in August, a book will come out which is called “The First Survivors of Alzheimer’s.” I was excited to do this with seven survivors including Julie, who has a wonderful story, and all seven people wrote their first person stories about what it was like to be told that things were not good. What it was like as Julie was told, “Good luck with that.” Just horrible, and then to come back and do so well. So thank you very much, Julie for the fantastic story that you wrote for that book. And we go through some of the things that all of these various people did, to do, as well as they’ve done Sharon here says I did 23andMe but didn’t see any information on ApoE4. So yes, there’s a little Alzheimer’s section you’ll need to check that you want to see this, and you’ll be able to see five different genes that include APOE. So it’s certainly a good thing and again, everyone should know this, everyone should get on appropriate prevention that is appropriate for your genotype and your haplotype. Maria says, let’s see, you can also upload data from 23andMe to Promethease. Yes, very good point and Julie’s talked about that before. Danielle says I have one good copy of SRT1 And this goes back to Ram’s very exciting work for a few years ago. Does the APOE4 status take away from its protective nature? Well, as Ram found in the brains, you will see a reduction in the overall SRT1, but that doesn’t mean that it won’t help you to have a copy of the good SRT1. Christine says, is there such thing as too low fasting insulin levels? Great point, Christine and we did write about that in “The End of Alzheimer’s Program,” with Julie and with Aida. And as long as you are getting appropriate insulin activity that is to say your hemoglobin A1C is good, you want to see it around 5.0, or a little lower or slightly higher, but you don’t want to be up at 5.5, six, seven, or eight, where you’re getting into pre-diabetes. And as long as your HOMA-IR is good, if your fasting glucose is 120, then having a low insulin is… So you can see there are two reasons to have a low insulin. One is your pancreas just ran out of the ability to make it and now you’re developing diabetes, that’s the bad way to have it, the good way to have it is you’re so insulin-sensitive that you’ve got a good fasting glucose, a good hemoglobin A1C and your fasting insulin can do all this even though it’s at 1.5 or 2. So I will usually look at when we’re treating people to make them better, if they have a lot of insulin, fine, we can bring that down. If they have none, and they’re very low and their glucose is very high, then I realize they basically, they become exhausted in the ability to make it. Now what happens is as they get on the right protocol, they get healthier, their fasting insulin will now actually start to come up a little because they can make an appropriate amount. So, very good question from Christine. Danielle, so here’s a good one for Julie. Danielle says, I thought moderate consumption of red wine was beneficial?
Julie Gregory: Right, that’s what the research shows if you’re not an ApoE4 carrier, but it doesn’t mean as an ApoE4 carrier that you have to completely abstain, consider doing something like dry red wine from Dry Farms, very low alcohol, low sugar, organic in small amounts. Try to stick to four ounces or less, once in a while.
Dr. Rao: Yeah, on that note, actually, see one of the things why people get attracted to red wine is because of SRT1. I mean, that’s, that’s what they said, SRT1 present in the red wine promotes all the good things. Now that the thing is, if it’s just for SRT1 thing you don’t necessarily have to take red wine. I mean SRT1 levels can go high with so many other things. We know that from other people’s research that fasting, prolonged fasting like 14 to 16 hours or physical exercise, mental exercise all these are known to increase the SRT1 level. So the same benefits that you get from red wine you get the same benefits from doing all the other associated activities. So, and you still get the benefits of it because SRT1 levels are going high, BDNF is going high, so you get the same benefits doing other activities as well.
Dr. Bredesen: Yeah, good point. So the next one Karen says, just saw the podcasts by Dr. Joel Kahn that cited a study saying that 16 hour plus fast showed more muscle attrition. So atrophy, there’s sarcopenia basically than 12 hours, is this correct? So this is, I think a really good point that we find again and again and again, people who are able to get feedback and kind of adjust for themselves are the ones that are doing the best. I know Julie, you’ve done a great job with this, looking at what things are helping, what things are not helping. So this is because the human organism is very complex. So you need to get this true. Some people, especially those who are getting poor uptake they’re poor absorption, which happens to many of us as we get older of proteins are going to have more sarcopenia. So they may need to be on digestive enzymes, they may need to be on some Betaine HCL. They need that may need to have a little higher protein in their diets. So you want to adjust, yes if you’re getting some sarcopenia, now how much do you have to fast? Well, please check your ketones and you’ll find out, you may want to adjust it. Some do very well with 18 or 20 hours, some people want to be down more like 12 or 13 hours. So it depends on your APOE status, it depends on your ability to absorb protein, on your diet, on your ketone level. You can adjust all these things so that you get the best outcomes. But of course, yes, there are going be some people that as they go to a longer and longer fast, no surprise they’re going be at increased risk for sarcopenia. So, Julie, how did you end up with your current status with the amount of fasting you do?
Julie Gregory: I think that Karen brings up a really good point and that’s why we recommend strength training at least for three to four times a week. I do KAATSU every day I feel so much better after I do it. It’s a special form of strength training. I also do aerobic exercise for over an hour a day, just walking or running outside. So when you’re doing this long, extended fast you need to make sure that your muscles are staying strong, you’re doing weight bearing exercise and as you mentioned, you’re getting enough protein and also that you’re maintaining a healthy weight.
Dr. Bredesen: Yeah, and then Sarah asks, I had 23andMe done in 2015. Would they flag APP if I had it? So they will not flag it for you, you’re going have to go in there and check it. And there was that period where they weren’t allowed to report it because of the FDA but they’re now once again, allowed to report it. So you should be able, if you had it done you should absolutely be able to know your APOE status. And then Linda asks, do you have suggestions for a person who is ApoE3/4, so single copy, also has histamine intolerance that causes hives and severe migraines, can’t eat many of the healthy recommended foods without problems such as avocados, sardines, mackerel, nuts, etc. trying to avoid histamine foods, grains, dairy while trying to gain weight, very low BMI. And I think this is a really good point that you brought up Linda. And we did talk a talk about this in “The End of Alzheimer’s Program.” And Julie wrote extensively about this as well as Aida because this is an issue. There are two separate issues here, one is the histamine issue and the other one is the issue of low BMI. No question, it is tougher when you start with a low BMI the people who have a little extra, they can lose some weight and it’s no problem, the people who are already at the low end really have to cycle. You have to go, you’re out of it, you’ve got to get a little more liberalized once or twice a week. Otherwise you can actually go backwards because you just don’t have enough energy and energetics part of the overall program. So, Julie, what do you recommend to someone like Linda who’s got both an issue with histamine and an issue with low BMI.
Julie Gregory: You know, I used to suffer from mast cell activation, so I feel for you, it’s very frightening. I used to get anaphylaxis and I had no idea what was triggering it, so it was really scary. I think that a lot of what helped me heal was focusing on gut health, focusing on leaky gut and cleaning up diet in general. But I would invite you to come to the apoe4info forum and we can have a longer conversation about that because it’s very complex to treat.
Dr. Bredesen: Yeah, and please take a look at what Julie wrote in the book “The End of Alzheimer’s Program,” ’cause she’s got an excellent section on that. Then Wendy asks, if we travel overseas is it okay to eat some grains or breads? And this of course gets back to some of the more ancestral grains and breads. And what do you suggest for that? Although ancestral, it’s still not 10, 20, 30,000 years ago or a million years ago, that sort of thing but it’s not within the last few hundred years. And so talk a little bit about what about people who are traveling.
Julie Gregory: It’s certainly a cheat for sure. I mean, and if you’re in Italy and you want to try some pasta or bread, I mean go ahead and try it and see how you feel and be consciously on the lookout for symptoms. I know Dr. Gundry recommends that his patients, when they travel, especially to Europe, go ahead and enjoy, the grains there in moderation, paying attention to how you feel.
Dr. Bredesen: Yeah, great point. Okay, the next one is from Marge, who says do you recommend exosome therapy for someone who has the ApoE4/4 who already has MCI, AMCI it says here. So presumably an amnestic MCI which is what’s usually meant by AMCI also dealing with neuro Lyme and mold infection. So this is, I’m really glad you brought this up Marge because this comes up all the time. There are all the, there are continuing new things and so what we recommend is please don’t give up. So many people will say, “Well I’ve been told “that there’s nothing you could do, “I tried something for a month or two, “it didn’t really seem to help me and so I’m giving up now.” Please don’t give up, there is so much. I heard a marvelous story last week, nice documentation of improvement in someone who has a completely untreatable disease that has been called PSP where there are some improvements with stem cells. So please don’t give up, the arsenal is growing, so what we recommend get on the basics, do the basics, do the diet, the exercise, sleep, stress, the brain training, but supplementation, the detox. Do the basics, get yourself into mild ketosis. Make sure there’s not inflammation, make sure your gut is healed, check your oral DNA, check your SPO2 at night, do all the basics, and then see where you stand. If you haven’t addressed things optimally, then absolutely there are the plasmalogens that were mentioned by Julie, plasmapheresis, there’s a group now reporting some good results with plasmapheresis. There are multiple groups doing stem cells. You mentioned the exosomes here. Exosomes are fascinating because they are bi-directional, your brain creates these exosomes, which are tiny, tiny little particles that come from your cells, there are 1.2 billion of these for each milliliter of your blood. It’s amazing, so these things are communicating, just like we think of the gut and brain access, there’s the exosome brain blood access, where these things are being produced in your brain but they’re also going back into your brain. So absolutely it’s going to be one of the things for the future, you have to say it is still an experimental approach, but something to consider after you’ve done all of the basics absolutely. So the next one here is from OG, who says which EWOT company, and again, we’re agnostic to whatever works the best, we have in the past recommended LiveO2 because it’s one that actually will cycle you from hyperoxia slight hypoxia which gets kind of the best of both worlds, but also MaxO2 makes a very good machine. So there are multiple ways you can go there with EWOT and certainly something that can give appropriate oxygenation. There’s a group out of Israel reporting very good results with another approach which is HBOT, which is hyperbaric oxygen where they also do the cycling in theirs. And they believe that that cycling is an important piece of this. And then Sandra asks on omega-3 subject, what about algal oil supplementation? We like it, causes less burping and indigestion, does system need to be changed in the fish gut? No, that’s a very good point. And the algal tends to have more of the DHA which is the longer chain and a little less of the EPA which often is a good thing. So please again, you can close the circle check at the other end ultimately what your omega-3 ratio is check to see where your DHA and EPA are. And Ram, have you used with your Ayurvedic practice, do you ever recommend algal oil to people?
Dr. Rao: Yes, absolutely for people who did not take seafood, so it’s two things that interesting here. Number one I would always say is, they don’t say no to meat and seafood, but when it comes to seafood, they always say, go to the ocean and then go to the middle of the ocean and then use the seafood for that is the present in the middle of the ocean. So they knew that anything that is in the shore would be contaminated. So they always said, so two things there. They said they can add extra effort to go to the ocean, so naturally, you know you have to paddle, those days there are were machine boats, it was easier to paddle. So which means exercise and then exercise combined with fishing in the middle of the ocean. So number one was ocean-based of seafood, they said for people who couldn’t stand that we always, they took the sea vegetables, what we call sea vegetables, and then extracted the oil from there and then that’s what they were giving to all the people. And that’s what they do even in the retreats. They give these algal-based oils to these people.
Dr. Bredesen: Yeah, great, okay, good points. And then Julie, Ellen here said two things, what’s your thought on soy products and how about MCT oil for people with APOE4? And I think this is a great point because this comes up all the time.
Julie Gregory: Right, let me start with the MCT oil, so that’s high in saturated fat. So if you need an exogenous source of ketones if you’re insulin resistant and you can’t create your own ketones through fasting, exercise and diet, maybe consider ketone salts or esters instead of MCT. And I think soy is a great source of complete protein especially for vegans. I think that there have been some health concerns that are probably overstated (and we take a pretty deep dive into this in the book) and there’s probably some health benefits about soy that had been overstated as well, but it’s a great source of complete protein for vegans for sure.
Dr. Bredesen: Then Bill asks, my mother had early onset Alzheimer’s and I carry APOE4, what should I do next? So I was so glad you brought this up because this is a great point and as I mentioned earlier, there are 75 million Americans who have a single copy of ApoE4 and the vast majority unfortunately don’t know about it and don’t find out about it until they actually have problems down the road. So this is exactly why we created PreCODE, which is for prevention of cognitive decline. If you are asymptomatic, very simple and easy to do, please check, you can go on online to Apollo Health Co or you can go to My Cognoscopy or you can go to PreCODE and simply get some simple blood tests. So you can see where you stand. It will give you step-by-step instructions because you should stay sharp to a hundred. We should be able to make Alzheimer’s a very rare disease by having everyone get on appropriate prevention or at the latest, early reversal. It’s the ones who wait and wait and wait, because a window is actually quite large but don’t wait until you’re so far along that it’s much more difficult to do. So please, Bill, you should be able to stay sharp until you’re a very ripe old age. Sean asks, how does one accurately differentiate between type 1.5, which is the glycotoxic with people with insulin resistance and physiological insulin resistance or adaptive glucose sparing commonly seen in those eating and of Alzheimer’s program, KetoFLEX 12/3 diet. So this is a good point that there is a difference here in that when you have type 1.5, number one, you are having some cognitive issues by definition when you have type 1.5, so you have cognitive changes and then you typically will have insulin resistance, your HOMA-IR will be high. We like to keep it down at one, 1.0, 1.1, 0.9 right in that area. If you’re up at two, three, these are very high HOMA-IRs and you could get that very simply fasting blood sugar times, fasting insulin divided by 405, easy to do on your iPhone in two seconds and you can see what your HOMA-IR actually is. Now you’re right there over time, some people, and Julie, you wrote about this in the book, they will creep up a little over time but they won’t have the high HOMA-IRs, they won’t have the changes in brain function. So what do you say to people who are saying, yeah, I’ve been on a KetoFLEX 12/3 diet for a while and I’m seeing that my glucose is creeping up a little bit over time.
Julie Gregory: Right, I’ve been chatting with Sean about this through private messaging and he brings up a really good point. He says that his HOMA-IR wouldn’t be that good considering the physiological insulin resistance. So for people like Sean who have the higher fasting glucose in the morning, what do you think about doing that test with the glucose later in the day? You know, we have to imagine there’s some dawn phenomenon going on. This particular guy has the physique of someone who’s very insulin sensitive. Yet the high fasting glucose in the morning is concerning.
Dr. Bredesen: So one thing I would do if I had a high fasting glucose in the morning, I would be very careful about looking at what’s going on with sleep. You could have adrenaline going on, you could have upper airway resistance syndrome, you may have a little bit of sleep apnea that you’re not aware of. You may be dropping your oxygenation. Something is pushing that up where it sounds like the rest of things are very good for you. So I would be, I would look into further what’s going on while you’re sleeping, because that may be one of the things that’s pushing this problem. And there’s a comment here from Dan, let’s see here. It says thanks for the broadcast, even after reading the books, I learned a lot. Great, thank you, Dan. He said he loved Ram’s comment about ApoE4 the right genes in the wrong environment. So yeah, very good point. And thank you very much for that, Dan. Let’s see, let’s see here. What’s the best exercise for carriers of the gene, is there a type of exercise that would not be good for carriers? I’m a long distance runner and can easily run 20 plus miles on a good day, but I wonder if that’s inflammatory. Such a good point and I’m glad you brought that up because this is another thing that comes up a lot. So the phenomenon of hormesis, is where we push ourselves a little bit and now our bodies respond. Hormesis is a thing that actually can be helpful to us. Again, our systems have an area they’re meant to function, when we push them a little, the good news is we’ll now respond. We’ll be stronger, it’s why people work out, it’s why people run, all these things. Unfortunately, there is a curve there and you now push it too much then you’re actually hurting things. And yes, people who run repeated marathons can break down. They can have problems with arthritis, they can have problems with bone damage, with ligament damage on and on. So yeah, it’s a good point, I think people more and more are recognizing you just can’t push it. Remember that the guy who ran the very, very first marathon died at the end of that. So back in the Greek days, so please be careful when you’re out there. And we probably should be doing a little bit less than that quite, especially on a repeated basis. So, Julie, what do you recommend about where is, I know you get out in the cold and you get out there and running and hiking what’s too much?
Julie Gregory: You know, when I learned about my ApoE4 homozygote status, I looked at exercise differently because I was a lot like this gentleman, I like to push myself. I was in bootcamp style classes, I was always trying to do the fastest mile and beat my personal best but once I learned that I’m so pro-inflammatory, I started taking exercise a little easier. But so yeah, I’m out there for an hour, hour and a half walking. I run for some, I walk for some, but I do hill work, I challenge myself. I mean, so I wouldn’t push it for repeated running for 20 miles, I think, especially as a homozygote I think that’s probably too stressful, too pro-inflammatory. But I also think, and I mentioned this earlier that strength training is extraordinarily important. If I don’t strength train on a regular basis my cognition feels different. I feel less sharp.
Dr. Bredesen: Interesting comment here from Dan who says, great question, Brady, he goes back to the long-distance running issue and he says he’s now gotten off that simple cards such as Gatorade and Cliff Bar’s for long distance training. Interestingly, what he says is he’s lost weight, he’s slightly faster now with his running than he was 10 years ago. Fantastic, this is so great to hear Dan. So you’re obviously doing the right things. Sharon says, does MCT oil in black coffee take me out of fasting? That is a great point and it’s certainly the good news is it doesn’t take you out of ketosis. The usual rule is if you stay under 50 calories you can typically stay in a fasting-like state. However, it depends a little bit therefore how much you actually put in there. whether you’re going to come out of your fasting state. But the good news is, it’s not a glycemic load, you’re not giving yourself sugar. So you’re still going to keep yourself into ketosis. And then what do you tell people, Julie about people who are going be using things like MCT oil in their coffee?
Julie Gregory: I would encourage Sharon to create her own endogenous source of ketones by just extending that fast, by exercising while you’re fasting and by adopting our version of the diet (KetoFLEX 12/3), you can get into the same level of ketosis without any exogenous sources of ketones, like MCT. So that’s the ancestral way of doing it, it’s healthy and you can just naturally create your own ketones. That’s what our ultimate goal is.
Dr. Bredesen: And, going back to Brady’s point earlier about what’s the best exercise, I would encourage Brady, please check out some KAATSU bands. And more and more people are saying, wow, we’re really getting some interesting effects. I know elderly people who are very elderly are claiming very good effects. We had a very interesting follow-up this week from someone who is unfortunately has very high amyloid load and was saying, wow, I’m doing much better with the KAATSU bands in addition to the rest of the program. So I think they’re beginning to suggest that these things could be very, very helpful. I know you’ve had very good luck with them yourself. And then Sean asks, what tests do you prefer? Omega-3 levels and Omega-3 to 6 ratio. Yeah, so I think either one is fine. I like to see the six to three ratio and you want to keep it down. If you can keep it at two or three or four, not 10 or 12 or 15, that’s great, but also helpful to have the omega-3 index where you want to be up at the 10% or so, if you’re APOE4, you want to be 10 or above. If you’re APOE4 negative, you still want to be somewhere around 10 or so. And then Christine asks, can you suggest how many tablespoons of fat someone should have a day? What does 10% of fat look like? Okay, so yeah, I always liked Cronometer I think to go back to look to see what kind of fats you’re taking in that is so helpful but it’s a free thing you can do online, it’s easy. You can see if you’re getting enough, various nutrients. I was surprised to see how badly I was doing with choline when I started looking at it. I was also surprised to see that, yes I tended to be too high on the carbs and too low on the fats and proteins. So I would need to adjust for that. So I think that it’s an easy thing to do, lots of people using it and I know Julie, you’ve talked about it in the book as well. So there’s one final here, which is on a blood type. This is a good point. No question, the people who have more trouble with COVID are people who are male, who are overweight who have many of the same risk factors for Alzheimer’s disease and who are blood type A, who have hypertension, who have any clotting issues who have insulin resistance, who have low vitamin D level, low zinc, many of these same risk factors. I’m not aware that that blood type A has been an issue with respect to Alzheimer’s disease. So I think that’s something that’s more seems to be COVID related. But Ram and Julie, you may know different in terms of blood type A and a risk for Alzheimer’s disease.
Dr. Rao: No, haven’t talked about that.
Dr. Bredesen: Okay, certainly, as we talked about last time here, having APOE4 is a problem with increased risk for poor outcomes from COVID. And so please, we’re hearing more and more about the long haulers and effects on brain. So please everyone stay safe, please be careful out there. Please keep your social distancing and let’s all stay healthy. And please everyone get on appropriate prevention or earliest reversal, so everyone can stay sharp till a hundred. Thank you very much, Julie, thanks very much Ram, great to talk with everyone and thanks for the excellent questions. – Thank you.




